Acute-on-Chronic Liver Failure
Summary
Acute-on-chronic liver failure (ACLF) is a distinct syndrome characterised by acute hepatic decompensation in patients with chronic liver disease (typically cirrhosis), leading to organ failure(s) and high short-term mortality. The EASL-CLIF Consortium definition requires: (1) acute decompensation of cirrhosis (ascites, encephalopathy, GI bleeding, infection), (2) organ failure (defined by CLIF-SOFA score), and (3) high 28-day mortality. ACLF differs from simple decompensated cirrhosis by the presence of systemic inflammation and multi-organ dysfunction. Common precipitants include bacterial infection (40%), active alcoholism, and GI bleeding. Early identification of precipitant, aggressive supportive care, and liver transplant evaluation are cornerstone of management.
Key Facts
- Definition: Acute decompensation + organ failure(s) + high short-term mortality in cirrhotic patients
- Incidence: 20-35% of hospitalised cirrhotic patients meet ACLF criteria
- Mortality: 28-day mortality: Grade 1: 22%, Grade 2: 32%, Grade 3: 73%
- Peak Demographics: 50-65 years; alcohol-related cirrhosis most common aetiology
- Pathognomonic: Systemic inflammatory response with multi-organ failure
- Gold Standard Investigation: CLIF-SOFA score for grading
- First-line Treatment: Treat precipitant + organ support + transplant evaluation
- Prognosis: Potentially reversible if precipitant treated early; otherwise rapidly fatal
Clinical Pearls
Diagnostic Pearl: All hospitalised cirrhotic patients with acute decompensation should be assessed for organ failures using CLIF-SOFA to identify ACLF.
Treatment Pearl: Infection is the most common precipitant (40%) - have low threshold for empirical antibiotics and thorough infection screen.
Pitfall Warning: Distinguish ACLF from simple decompensation - prognosis and management intensity differ markedly.
Mnemonic: ACLF ORGANS - Acute precipitant, Cirrhosis underlying, Liver failure, Failure of other organs, Organ support needed, Really high mortality, Grade by CLIF-SOFA, Assessment for transplant, Need to act fast, Severe inflammation
Why This Matters Clinically
ACLF represents a paradigm shift in understanding cirrhosis - from chronic progressive disease to acute critical illness requiring intensive care. Recognition enables appropriate level of care, prognostication, and early transplant evaluation. This is increasingly examined in MRCP and acute medicine contexts.
Incidence
- 20-35% of hospitalised acute decompensation patients meet ACLF criteria
- Annual incidence in cirrhotic population: 10-15%
- Increasing recognition with standardised definitions
Risk Factors
| Factor | Impact |
|---|---|
| Alcohol-related cirrhosis | Higher ACLF incidence |
| Active drinking | Common precipitant |
| MELD score >15 | Increased risk |
| Prior decompensation | Increased susceptibility |
| Bacterial infection | Most common precipitant |
Mechanism
Step 1: Chronic Liver Disease (Cirrhosis)
- Established cirrhosis with portal hypertension
- Reduced hepatic reserve
- Immune dysfunction (cirrhosis-associated immune dysfunction - CAID)
Step 2: Precipitating Event
- Bacterial infection (most common 40%): SBP, UTI, pneumonia, cellulitis
- Alcoholic hepatitis
- GI bleeding
- Drug-induced liver injury
- Viral hepatitis flare (HBV reactivation)
- Surgery, TIPS
Step 3: Systemic Inflammatory Response
- Massive cytokine release (IL-6, IL-8, TNF-α)
- Pathogen-associated molecular patterns (PAMPs) from gut translocation
- Damage-associated molecular patterns (DAMPs) from hepatocyte necrosis
- Systemic inflammation disproportionate to precipitant
Step 4: Multi-Organ Failure
- Liver: Hyperbilirubinaemia, coagulopathy, encephalopathy
- Kidney: Hepatorenal syndrome, ATN
- Brain: Hepatic encephalopathy
- Coagulation: DIC-like pattern
- Circulation: Vasodilatory shock
- Respiratory: ARDS, hepatopulmonary syndrome
Step 5: Outcome
- Reversible if precipitant controlled and organs supported
- Without transplant in severe cases: death within days-weeks
- ACLF Grade 3 mortality 73% at 28 days
Classification (CLIF-SOFA/EASL-CLIF)
| ACLF Grade | Definition | 28-day Mortality |
|---|---|---|
| No ACLF | No organ failure or single non-kidney failure | 5% |
| Grade 1 | Kidney failure alone, OR single organ + kidney dysfunction | 22% |
| Grade 2 | 2 organ failures | 32% |
| Grade 3 | 3+ organ failures | 73% |
Organ Failure Definitions (CLIF-SOFA):
| Organ | Failure Criteria |
|---|---|
| Liver | Bilirubin ≥204 μmol/L (12 mg/dL) |
| Kidney | Creatinine ≥176 μmol/L (2 mg/dL) or RRT |
| Brain | Hepatic encephalopathy grade 3-4 |
| Coagulation | INR ≥2.5 |
| Circulation | MAP less than 70 or vasopressor requirement |
| Respiratory | PaO2/FiO2 ≤200 or SpO2/FiO2 ≤214 |
Symptoms
Signs
Red Flags
[!CAUTION]
- Grade 3-4 encephalopathy
- Hypotension requiring vasopressors
- Renal failure (urine output less than 0.5ml/kg/hr)
- Respiratory failure
- Multi-organ involvement
Assessment
General:
- GCS, orientation
- Jaundice severity
- Signs of sepsis
Cardiovascular:
- MAP less than 65 concerning
- Hyperdynamic circulation typical
Abdominal:
- Ascites (shifting dullness)
- Hepatomegaly/splenomegaly
- Tenderness (SBP if present)
Neurological:
- Hepatic encephalopathy grading (West Haven)
First-Line
- LFTs: Bilirubin, INR (liver failure assessment)
- U&E: Creatinine (kidney failure)
- ABG: Lactate, respiratory function
- Infection screen: Blood cultures, urine, ascitic tap
Laboratory
| Test | Purpose |
|---|---|
| Bilirubin | Liver failure criterion |
| INR | Coagulation failure |
| Creatinine | Kidney failure |
| Lactate | Tissue perfusion |
| WCC, CRP | Infection |
| Ammonia | Encephalopathy |
| Ascitic fluid | SBP screen (PMN >250) |
Imaging
| Modality | Purpose |
|---|---|
| CXR | Infection, respiratory failure |
| USS Abdomen | Ascites, portal vein, hepatic veins |
| CT if indicated | Exclude other pathology |
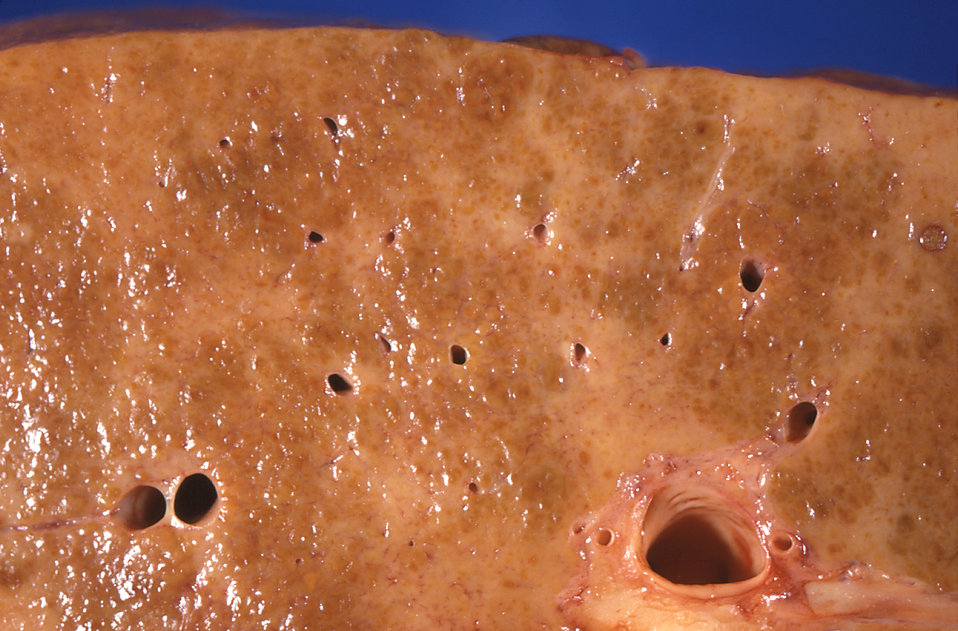 Gross pathology of cirrhotic liver. Source: Wikipedia Commons (CC0)
Gross pathology of cirrhotic liver. Source: Wikipedia Commons (CC0)
Algorithm
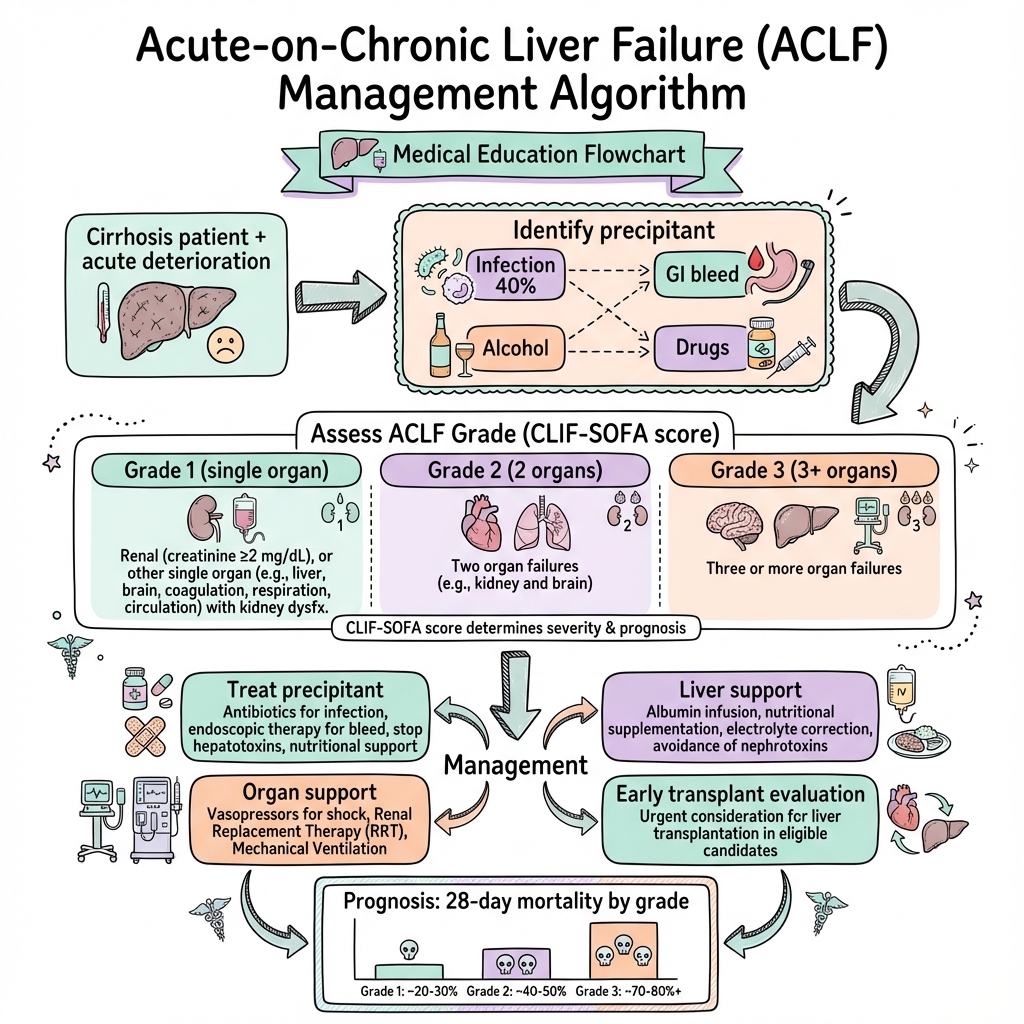
Immediate Management
- ABC assessment
- Resuscitation (cautious fluids)
- Identify and treat precipitant
- Calculate CLIF-SOFA grade
Treat Precipitant
| Precipitant | Treatment |
|---|---|
| Infection/SBP | IV ceftriaxone + albumin |
| Alcoholic hepatitis | Steroids if DF >32, no infection |
| Variceal bleed | Terlipressin, endoscopy, antibiotics |
| Drug-induced | Stop offending agent |
| HBV reactivation | Tenofovir/entecavir |
Organ Support
Liver Support:
- Nutrition (high protein if no encephalopathy)
- Lactulose for encephalopathy
- Rifaximin
- Avoid nephrotoxins, hepatotoxins
Kidney:
- Albumin infusion (1g/kg) if Type 1 HRS
- Terlipressin + albumin for HRS
- RRT if refractory
Circulation:
- Noradrenaline if vasopressor needed
- Judicious fluids (avoid volume overload)
Respiratory:
- Oxygen, NIV, intubation as needed
- Treat underlying cause
Coagulation:
- FFP/platelets only for active bleeding or procedures
- Vitamin K
Transplant Evaluation
- Early referral for ACLF Grade 2-3
- Contraindications assessed (infection, active alcohol)
- Futility assessment for Grade 3 with no improvement at 3-7 days
Disposition
- ICU: ACLF Grade 2-3, organ support needed
- HDU: ACLF Grade 1, single organ failure
- Ward: No ACLF, decompensation management
| Complication | Incidence | Management |
|---|---|---|
| Multi-organ failure | 30-50% | ICU support |
| Sepsis | 40% | Broad-spectrum antibiotics |
| Hepatorenal syndrome | 20-30% | Terlipressin + albumin |
| Cerebral oedema | less than 5% | Mannitol, hypertonic saline |
| Death | 22-73% by grade | Transplant if eligible |
Mortality by Grade
| Grade | 28-day Mortality | 90-day Mortality |
|---|---|---|
| No ACLF | 5% | 14% |
| Grade 1 | 22% | 41% |
| Grade 2 | 32% | 52% |
| Grade 3 | 73% | 79% |
Prognostic Factors
Favourable:
- Identifiable, treatable precipitant
- Improvement in day 3-7 CLIF score
- Eligible for transplant
- Younger age
Unfavourable:
- No precipitant identified
- ACLF Grade 3
- No improvement by day 7
- Active alcohol use
- Contraindications to transplant
Key Guidelines
- EASL Clinical Practice Guidelines: ACLF (2023) — Comprehensive PMID: 36867091
- AASLD Practice Guidelines — American guidance
Landmark Studies
CANONIC Study (2013) — Defined ACLF criteria, CLIF-SOFA score. PMID: 23453491
PREDICT Study (2020) — Pre-ACLF identification. PMID: 32503680
What is ACLF?
When your liver disease suddenly gets much worse and other organs (kidneys, brain, lungs) also start to struggle. It needs urgent hospital treatment.
What causes it?
Often an infection, drinking alcohol, or bleeding. Finding and treating the cause is essential.
Treatment
Intensive care to support your organs while we treat the underlying problem. Some people need a liver transplant.
-
Moreau R et al. CANONIC Study: Acute-on-chronic liver failure. Gastroenterology. 2013;144(7):1426-1437. PMID: 23453491
-
European Association for the Study of the Liver. EASL Clinical Practice Guidelines on ACLF. J Hepatol. 2023;79(2):461-491. PMID: 36867091
-
Trebicka J et al. PREDICT Study: Pre-ACLF. J Hepatol. 2020;73(6):1454-1466. PMID: 32503680
-
Arroyo V et al. ACLF: A new syndrome. J Hepatol. 2015;62(1 Suppl):S131-S143. PMID: 25920085
-
Jalan R et al. Development and validation of CLIF-SOFA. J Hepatol. 2014;61(5):1038-1047. PMID: 24950482
Viva Points
"ACLF is acute decompensation of cirrhosis with organ failure(s) and high short-term mortality. Graded by CLIF-SOFA. Grade 3 has 73% 28-day mortality. Key management: identify precipitant (infection 40%), organ support, early transplant evaluation."
Key Facts
- CLIF-SOFA grading: Grades 1-3
- Infection is precipitant in 40%
- Grade 3: ≥3 organ failures, 73% mortality
- Early transplant referral essential
Common Mistakes
- ❌ Not calculating CLIF-SOFA in decompensated cirrhosis
- ❌ Missing infection as precipitant
- ❌ Delayed transplant referral
- ❌ Confusing with simple decompensation
Last Reviewed: 2026-01-01 | MedVellum Editorial Team