Adrenal Crisis
Summary
Adrenal crisis is a life-threatening emergency caused by acute cortisol deficiency that cannot meet physiological demands. It occurs in patients with primary adrenal insufficiency (Addison's disease), secondary adrenal insufficiency (pituitary failure), or tertiary insufficiency (chronic steroid suppression). The most common trigger is failure to increase steroid doses during illness, infection, or stress in a patient with known adrenal insufficiency. Key features include hypotension, hypoglycaemia, hyponatraemia, and altered consciousness. Treatment is immediate IV hydrocortisone - do NOT delay for investigations. Without treatment, adrenal crisis is rapidly fatal. Prevention through patient education and sick-day rules is essential.
Key Facts
- Definition: Acute cortisol deficiency with haemodynamic compromise
- Incidence: 5-10 crises per 100 patient-years in known adrenal insufficiency
- Mortality: 0.5% per crisis; 6% if hospitalised
- Common Triggers: Infection (most common), surgery, missed medications, trauma
- Pathognomonic: Hypotension + hyponatraemia + hyperkalaemia (primary AI) + hypoglycaemia
- Gold Standard: Clinical diagnosis - treat immediately, investigate later
- First-line Treatment: Hydrocortisone 100mg IV stat, then 50mg IV QDS
- Prognosis: Excellent if treated promptly; fatal if delayed
Clinical Pearls
Emergency Pearl: NEVER delay treatment for investigations. Give hydrocortisone 100mg IV immediately if clinical suspicion. Take random cortisol BEFORE steroids if possible (but don't delay for it).
Diagnostic Pearl: In primary AI (Addison's), expect hyperkalaemia due to mineralocorticoid deficiency. In secondary AI, potassium is normal.
Prevention Pearl: All patients on long-term steroids need sick-day rules and emergency injection training.
Why This Matters Clinically
Adrenal crisis is a preventable death. Every acute physician must recognise and treat immediately. Patient education prevents recurrence. This is a core MRCP and acute medicine topic.
Incidence
- 5-10 crises per 100 patient-years in known adrenal insufficiency
- Approximately 1 in 8 patients with Addison's will have a crisis per year
Causes of Adrenal Insufficiency
| Type | Causes |
|---|---|
| Primary (Addison's) | Autoimmune (80% in developed countries), TB, adrenal haemorrhage/infarction, metastases |
| Secondary | Pituitary disease, pituitary surgery, Sheehan syndrome |
| Tertiary | Chronic steroid use (most common overall) |
Triggers for Crisis
| Trigger | Frequency |
|---|---|
| Infection (GI, respiratory) | 40% |
| Missing/reducing steroid dose | 20% |
| Surgery/trauma | 15% |
| Emotional stress | 10% |
| Undiagnosed AI with first presentation | 10% |
Mechanism
Step 1: Baseline Adrenal Insufficiency
- Patient has primary, secondary, or tertiary AI
- Relies on exogenous steroids for cortisol replacement
- Basal requirements met, but no reserve capacity
Step 2: Stress/Trigger Event
- Infection, surgery, trauma, or illness
- Normal response: 10-fold increase in cortisol
- In AI: Cannot mount stress response
Step 3: Cortisol Deficiency State
- Loss of cortisol's permissive effects on vasopressors
- Impaired gluconeogenesis leads to hypoglycaemia
- Loss of negative feedback on ADH leads to water retention and hyponatraemia
- (Primary AI only): Loss of aldosterone leads to sodium loss, potassium retention
Step 4: Haemodynamic Collapse
- Profound hypotension unresponsive to fluids
- Circulatory failure
- Without treatment: Death
Primary vs Secondary AI
| Feature | Primary AI | Secondary AI |
|---|---|---|
| Aldosterone | Low | Normal |
| Potassium | High | Normal |
| Pigmentation | Present | Absent |
| ACTH | High | Low |
Symptoms
Signs
Laboratory Features
| Finding | Mechanism |
|---|---|
| Hyponatraemia | ADH hypersecretion + aldosterone loss (primary) |
| Hyperkalaemia | Aldosterone deficiency (primary AI only) |
| Hypoglycaemia | Impaired gluconeogenesis |
| Uraemia | Dehydration |
| Lymphocytosis, eosinophilia | Loss of cortisol effect |
Red Flags
[!CAUTION]
- Known AI patient with infection/illness
- Unexplained hypotension not responding to fluids
- Hyponatraemia with hyperkalaemia
- Patient on long-term steroids who is unwell
Assessment
General:
- GCS, confusion
- Hydration status
- Temperature
Cardiovascular:
- Blood pressure (hypotension)
- Heart rate (tachycardia)
Skin:
- Hyperpigmentation (palmar creases, pressure areas, buccal mucosa) - primary AI
Abdominal:
- Tenderness (may mimic acute abdomen)
Focus finding:
- Source of infection (chest, urine, abdomen)
Immediate (Do Not Delay Treatment)
If possible, take bloods BEFORE giving hydrocortisone:
| Test | Purpose |
|---|---|
| Random cortisol | Baseline (less than 100 nmol/L during stress = diagnostic) |
| ACTH | High in primary, low in secondary (if able to process) |
| U and E | Hyponatraemia, hyperkalaemia |
| Glucose | Hypoglycaemia |
| Blood cultures | If infection suspected |
After Stabilisation
- Short Synacthen test (when off steroids, stable)
- Autoantibodies (21-hydroxylase for autoimmune Addison's)
- Imaging if indicated (CT adrenals, pituitary MRI)
Algorithm
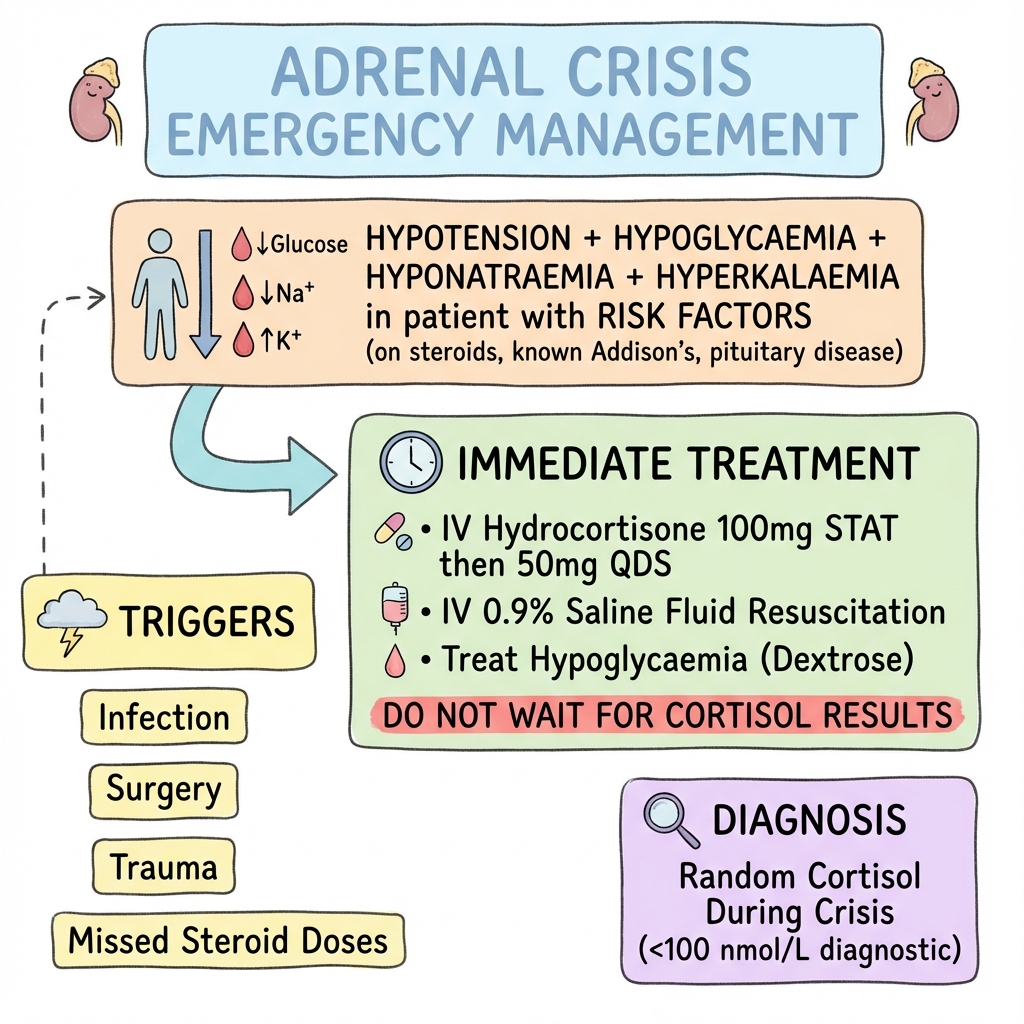
Immediate Management
Step 1: IV Hydrocortisone
- 100mg IV bolus IMMEDIATELY
- Then 50mg IV/IM every 6 hours (or 200mg/24h continuous infusion)
Step 2: IV Fluids
- 0.9% saline 1L rapidly
- Continue aggressive fluid resuscitation
- May need 2-4L in first few hours
Step 3: Correct Hypoglycaemia
- 10% or 20% dextrose if glucose low
Step 4: Monitor
- Urine output
- Electrolytes
- Glucose
- BP, HR
Step 5: Treat Trigger
- Antibiotics if infection
- Source control
Ongoing Management
Once stable:
- Convert to oral steroids when eating
- Hydrocortisone 20mg + 10mg + 10mg (or similar physiological dose)
- Add fludrocortisone if primary AI (100mcg daily)
Sick Day Rules (Prevention)
| Situation | Action |
|---|---|
| Fever, minor illness | Double oral steroid dose |
| Vomiting/diarrhoea | IM/SC hydrocortisone 100mg, seek help |
| Surgery | IV hydrocortisone cover |
| Major trauma | IM hydrocortisone 100mg, emergency services |
Patient Education
- All patients need:
- Steroid emergency card
- MedicAlert bracelet
- Emergency injection kit (IM hydrocortisone)
- Written sick day rules
- Education of family/carers
| Complication | Management |
|---|---|
| Cardiac arrest | Advanced life support + hydrocortisone |
| Cerebral oedema (from rapid Na correction) | Avoid overcorrection of sodium |
| Hypokalaemia (after treatment) | Monitor and replace |
Outcomes
- With prompt treatment: Excellent recovery
- Mortality per crisis: 0.5%
- Mortality if hospitalised: 6%
- Risk of recurrence: High if education inadequate
Key Guidelines
- Endocrine Society Guidelines (2016) — Diagnosis and treatment of primary adrenal insufficiency PMID: 26760044
- Society for Endocrinology Emergency Guidelines — Adrenal crisis
Key Studies
- Prevention studies showing patient education reduces crisis frequency
What is Adrenal Crisis?
Your adrenal glands cannot make enough cortisol, a hormone your body needs especially during illness or stress. When cortisol gets too low, it causes a dangerous drop in blood pressure and blood sugar.
How do you prevent it?
- Always carry your steroid emergency card
- Double your steroid dose when you are unwell
- Use your emergency injection if you cannot take tablets
- Never stop steroids suddenly
-
Bornstein SR et al. Diagnosis and Treatment of Primary Adrenal Insufficiency: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101(2):364-389. PMID: 26760044
-
Rushworth RL et al. Adrenal Crisis. N Engl J Med. 2019;381(9):852-861. PMID: 31461595
-
Hahner S et al. Epidemiology of adrenal crisis in chronic adrenal insufficiency. Eur J Endocrinol. 2015;172(5):R213-R220. PMID: 25800982
-
Arlt W. Adrenal crisis. Eur J Endocrinol. 2006;155(suppl 1):S91-S99. PMID: 17074715
Viva Points
"Adrenal crisis is acute cortisol deficiency with haemodynamic compromise. Treat immediately: hydrocortisone 100mg IV stat, then 50mg QDS, aggressive IV saline. Do NOT wait for investigations. Prevention: sick-day rules, emergency injection, MedicAlert."
Key Facts
- Hydrocortisone 100mg IV immediately
- Take random cortisol before steroids if possible
- Hyperkalaemia only in primary AI
- Most common trigger: infection
- All patients need emergency kit plus education
Common Mistakes
- Waiting for investigations before treating
- Forgetting to double dose during illness
- Not providing emergency injection training
Last Reviewed: 2026-01-01 | MedVellum Editorial Team