Acute Exacerbation of Bronchiectasis
Summary
An acute exacerbation of bronchiectasis is defined as a deterioration in respiratory symptoms requiring a change in treatment, typically antibiotics. The European Respiratory Society defines exacerbation as at least 3 of: increased cough, increased sputum volume or purulence, worsening dyspnoea, increased fatigue/malaise, fever, haemoptysis, or decline in lung function. Exacerbations drive disease progression, reduce quality of life, and increase mortality. Most are infectious, with Haemophilus influenzae, Pseudomonas aeruginosa, and Moraxella catarrhalis being common pathogens. Management centres on antibiotic therapy guided by sputum culture history, airway clearance, and adjunctive treatments.
Key Facts
- Definition: Deterioration in ≥3 respiratory symptoms requiring treatment change
- Incidence: 1.5-3 exacerbations per patient per year in moderate-severe disease
- Mortality: 2-4% per exacerbation; increased with Pseudomonas colonisation
- Peak Demographics: Bimodal - CF patients younger; non-CF bronchiectasis 50-70 years
- Gold Standard Investigation: Sputum culture + CXR
- First-line Treatment: 14-day oral antibiotics (guided by previous cultures)
- Prognosis: Frequent exacerbations predict accelerated lung function decline
Clinical Pearls
Diagnostic Pearl: Always send sputum culture before starting antibiotics - previous culture results guide empirical therapy in future exacerbations.
Treatment Pearl: 14-day courses are standard; 7-day courses have higher failure rates.
Pitfall Warning: Pseudomonas requires specific cover (ciprofloxacin or IV anti-pseudomonal) - standard amoxicillin will fail.
Mnemonic: BRONCH - Bacteria identification, Response assessment, Oral if mild, Nebulised therapy (if severe), Clearance (physiotherapy), Hospital if severe
Why This Matters Clinically
Exacerbation frequency is the strongest predictor of disease progression in bronchiectasis. Prompt, appropriate antibiotic therapy reduces exacerbation duration and prevents hospitalisation. Pseudomonas colonisation fundamentally changes management approach.
Incidence and Prevalence
- Exacerbation rate: 1.5-3 per patient per year
- Hospitalisation rate: 20-30% of exacerbations require admission
- Pseudomonas prevalence: 20-40% of bronchiectasis patients
Risk Factors for Exacerbation
| Factor | Impact | Management |
|---|---|---|
| Pseudomonas colonisation | 3x exacerbation risk | Eradication, suppression |
| FEV1 less than 50% predicted | Increased severity | Optimise therapy |
| Frequent exacerbations | Begets more exacerbations | Long-term antibiotics |
| Poor adherence to clearance | Sputum stasis | Physiotherapy review |
| Winter months | Viral triggers | Vaccination |
| Comorbidities (COPD, asthma) | Additive effect | Manage comorbidities |
Mechanism
Step 1: Bacterial Colonisation
- Structural airway damage permits chronic bacterial colonisation
- Biofilm formation in dilated airways
- Common organisms: H. influenzae, P. aeruginosa, M. catarrhalis, S. pneumoniae
Step 2: Trigger Event
- Viral infection, increased bacterial load, environmental trigger
- Shifts from stable colonisation to active infection
- Increased mucus production, impaired clearance
Step 3: Inflammatory Response
- Neutrophil-dominated inflammation
- Release of proteases (neutrophil elastase), cytokines
- Further airway damage - vicious cycle
- Systemic inflammatory response if severe
Step 4: Clinical Deterioration
- Increased sputum volume and purulence
- Worsening dyspnoea, cough
- Fatigue, possible fever
- Potential respiratory failure in severe cases
Step 5: Resolution or Progression
- With treatment: Symptom resolution over 7-14 days
- Without treatment: Risk of respiratory failure, sepsis
- Each exacerbation causes incremental lung damage
Symptoms
Signs
Red Flags
[!CAUTION]
- Haemoptysis >10ml
- SpO2 less than 92% on air
- Respiratory rate >25
- Signs of sepsis
- Confusion
- Failure of oral antibiotics
Structured Approach
General:
- Respiratory distress assessment
- Oxygen saturation, respiratory rate
- Temperature
Respiratory:
- Inspection: Use of accessory muscles, cyanosis
- Auscultation: Crackles (coarse), wheeze, bronchial breathing
Systemic:
- Signs of sepsis (hypotension, tachycardia)
- Nutritional status (CF/chronic disease)
First-Line
- Sputum culture (essential - guides therapy)
- SpO2 / ABG if hypoxic
- CXR (rule out consolidation, exclude other pathology)
Laboratory
| Test | Purpose |
|---|---|
| FBC | Leucocytosis, anaemia of chronic disease |
| CRP | Inflammatory marker, monitoring |
| U&E | Renal function for antibiotic dosing |
| Blood cultures | If septic |
Imaging
| Modality | Finding | Indication |
|---|---|---|
| CXR | New consolidation, mucus plugging | All exacerbations |
| CT Thorax | Extent of bronchiectasis | Not routine for exacerbation |
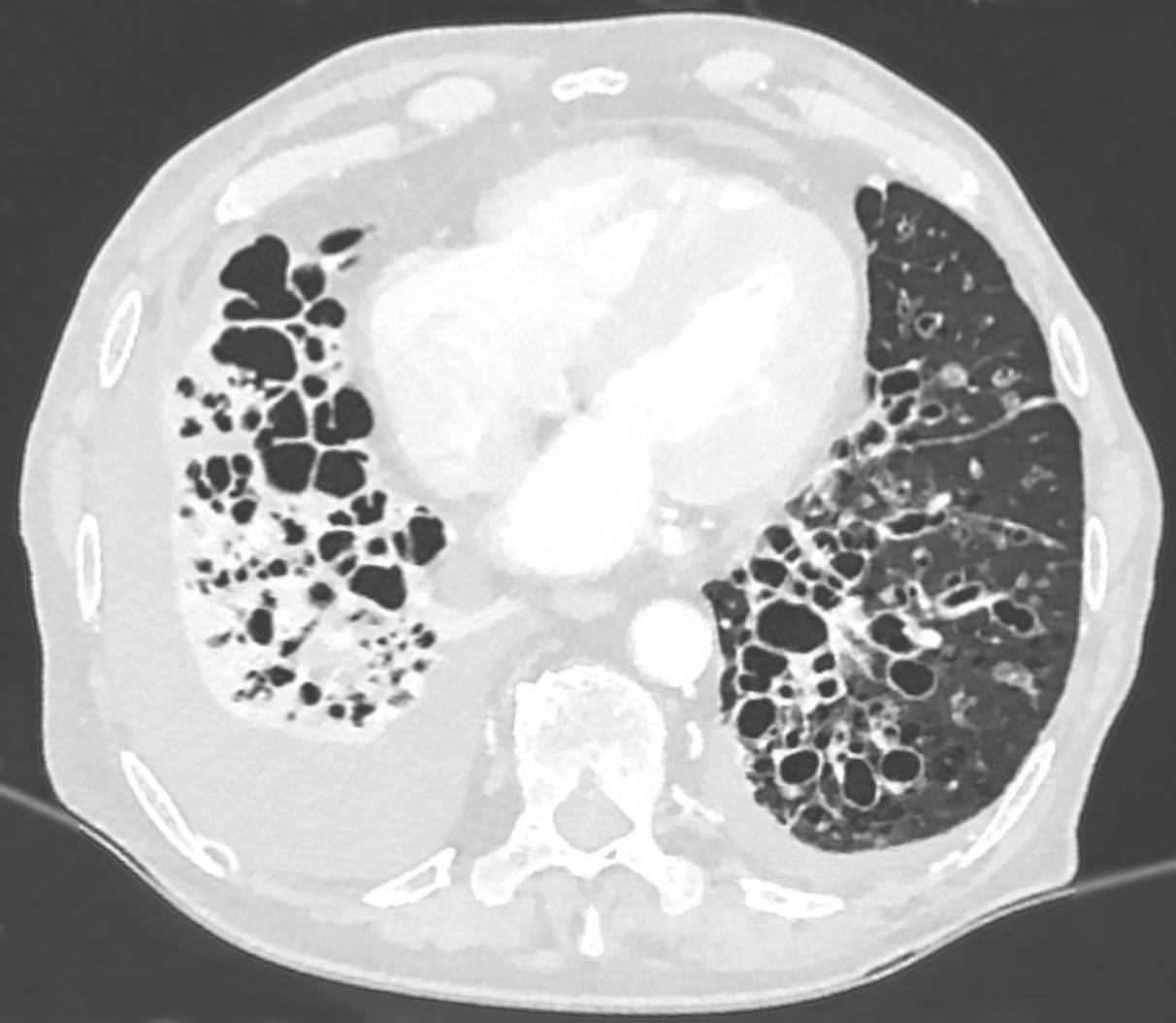 CT showing cystic bronchiectasis with dilated airways. Source: Wikipedia Commons (CC-BY-SA)
CT showing cystic bronchiectasis with dilated airways. Source: Wikipedia Commons (CC-BY-SA)
Algorithm
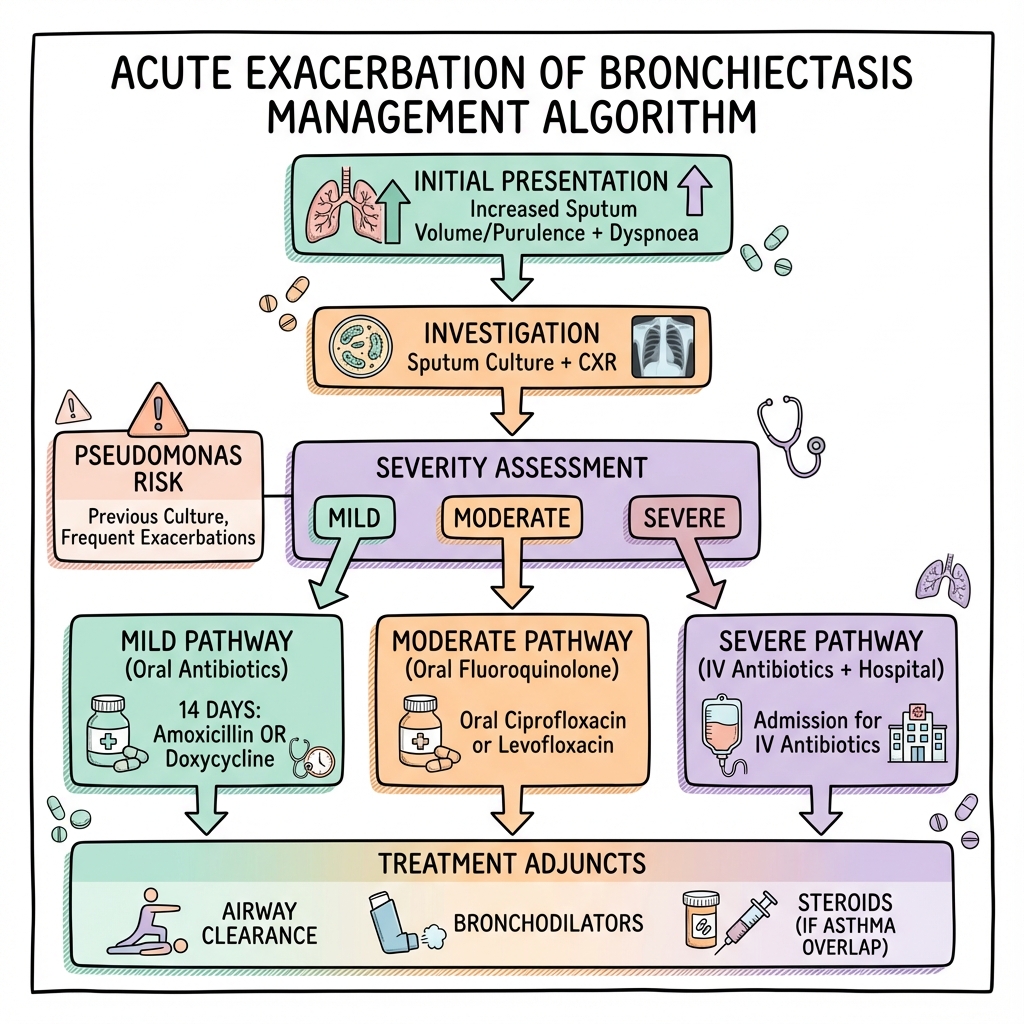
Assessment of Severity
| Severity | Criteria | Management |
|---|---|---|
| Mild | No systemic features, minimal change | Oral antibiotics, community |
| Moderate | Increased sputum, mild dyspnoea | Oral antibiotics, close review |
| Severe | Hypoxia, sepsis, failure of oral | IV antibiotics, admission |
Antibiotic Therapy
Duration: 14 days (evidence-based)
Choice Based on Culture History:
| Previous Culture | Oral Option | Alternative |
|---|---|---|
| H. influenzae | Amoxicillin 500mg TDS | Doxycycline 200mg then 100mg OD |
| M. catarrhalis | Co-amoxiclav 625mg TDS | Doxycycline |
| S. pneumoniae | Amoxicillin 500mg TDS | Clarithromycin 500mg BD |
| P. aeruginosa | Ciprofloxacin 750mg BD | IV if resistant |
| No prior culture | Amoxicillin 500mg TDS | Co-amoxiclav |
IV Therapy (Severe/Pseudomonas):
| Organism | Regimen | Duration |
|---|---|---|
| Pseudomonas | Piperacillin-tazobactam 4.5g TDS + Tobramycin | 14-21 days |
| Resistant Pseudomonas | Meropenem 2g TDS ± Colistin | Per microbiology |
| Empirical severe | Piperacillin-tazobactam | Until culture |
Adjunctive Therapy
- Airway clearance: Active cycle breathing, PEP devices, postural drainage
- Bronchodilators: Salbutamol if wheeze/bronchospasm
- Corticosteroids: Only if asthma/COPD overlap, not routine
- Mucolytics: Hypertonic saline, carbocisteine (adjunctive)
Disposition
- Admit if: Hypoxia, sepsis, failure oral therapy, significant haemoptysis, no home support
- Discharge if: Mild-moderate, improving on oral therapy, good support
- Follow-up: Respiratory clinic 4-6 weeks; review sputum culture results
| Complication | Incidence | Management |
|---|---|---|
| Respiratory failure | 5-10% of admissions | NIV, oxygen, ITU |
| Haemoptysis | 10-20% | Tranexamic acid, bronchial artery embolisation |
| Sepsis | 5% | IV antibiotics, source control |
| Development of resistant organisms | Variable | Antimicrobial stewardship |
Outcomes
- Exacerbation duration: 14-21 days typical
- Hospital mortality: 2-4%
- FEV1 decline: Accelerated with frequent exacerbations
- Quality of life: Significantly impacted by exacerbation frequency
Prognostic Factors
Good:
- Rapid response to antibiotics
- No Pseudomonas
- Good baseline lung function
Poor:
- Pseudomonas colonisation
- Frequent exacerbations (≥3/year)
- Low FEV1
- Multiple lobes affected
Key Guidelines
- ERS Guidelines on Bronchiectasis (2017/2024) — Diagnostic and management standards PMID: 28889110
- BTS Guideline for Bronchiectasis (2019) — UK practice recommendations PMID: 31413035
Key Evidence
EMBRACE Trial — Long-term azithromycin reduces exacerbations by 50% in frequent exacerbators. PMID: 22895560
BLESS Trial — Erythromycin reduces exacerbations. PMID: 23062527
What is a bronchiectasis flare-up?
A flare-up happens when your lung infection gets worse. Your lungs make more mucus that becomes thicker and yellower or greener. You feel more breathless and tired.
How is it treated?
You'll need antibiotics for 2 weeks. It's important to keep doing your airway clearance exercises to get the mucus out.
When to seek help
- Coughing up blood
- Severe breathlessness
- Fever not settling on antibiotics
-
Polverino E et al. ERS guidelines for the management of adult bronchiectasis. Eur Respir J. 2017;50(3):1700629. PMID: 28889110
-
Hill AT et al. BTS Guideline for bronchiectasis in adults. Thorax. 2019;74(Suppl 1):1-69. PMID: 31413035
-
Wong C et al. Azithromycin for prevention of exacerbations in non-cystic fibrosis bronchiectasis (EMBRACE). Lancet. 2012;380(9842):660-667. PMID: 22895560
-
Serisier DJ et al. Effect of long-term, low-dose erythromycin on pulmonary exacerbations (BLESS). JAMA. 2013;309(12):1260-1267. PMID: 23062527
-
Chalmers JD et al. The bronchiectasis severity index. Am J Respir Crit Care Med. 2014;189(5):576-585. PMID: 24328736
Viva Points
"Acute exacerbation of bronchiectasis is defined as deterioration requiring treatment change. Management is 14-day antibiotics guided by sputum culture history. Pseudomonas requires fluoroquinolone or IV therapy."
Key Facts
- 14-day course (not 7)
- Culture history guides empirical therapy
- Pseudomonas fundamentally changes management
- Airway clearance is essential adjunct
Common Mistakes
- ❌ 7-day antibiotic courses (inadequate)
- ❌ Ignoring previous sputum cultures
- ❌ Treating Pseudomonas with amoxicillin
- ❌ Forgetting physiotherapy
Last Reviewed: 2026-01-01 | MedVellum Editorial Team