IgG4-Related Disease
Summary
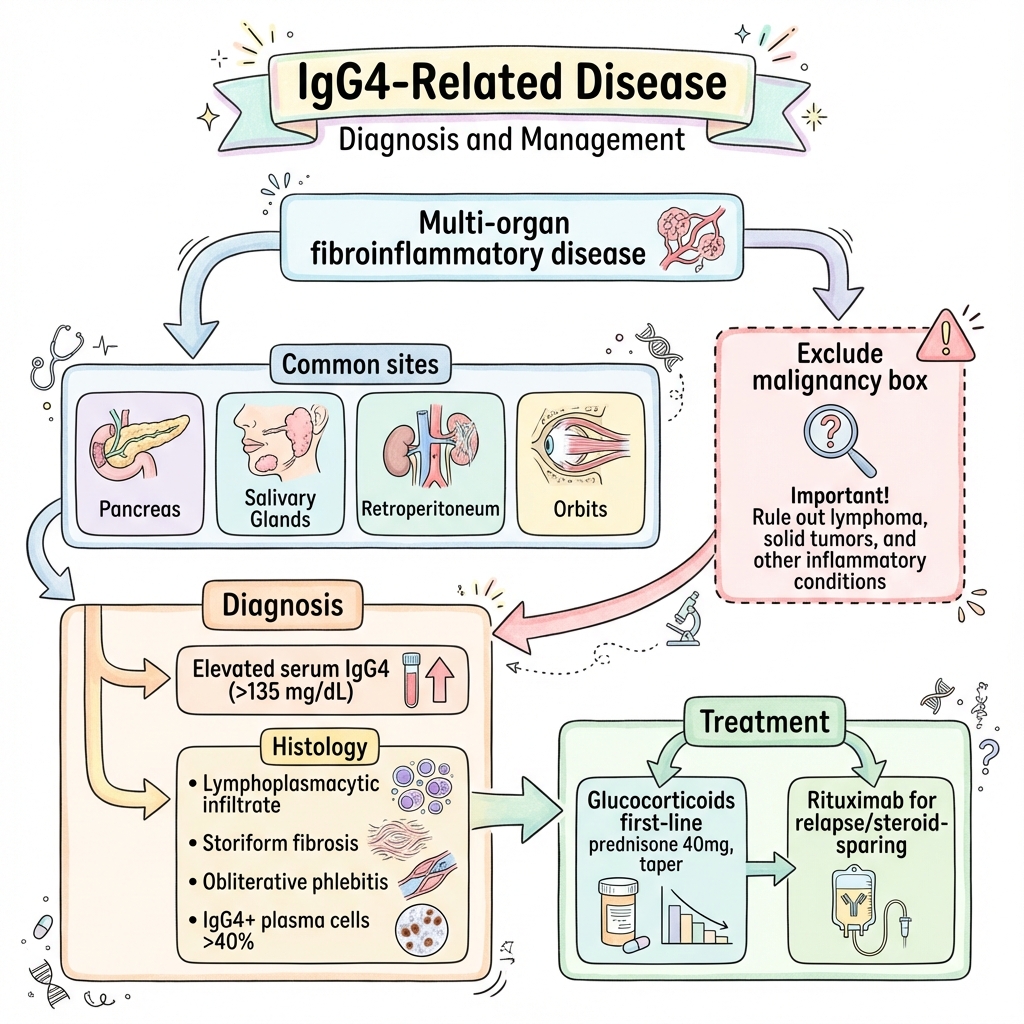
IgG4-related disease (IgG4-RD) is a fibroinflammatory condition characterised by tumefactive lesions, dense lymphoplasmacytic infiltrate rich in IgG4+ plasma cells, storiform fibrosis, and often elevated serum IgG4 levels. Previously recognised in individual organs (autoimmune pancreatitis, Mikulicz disease, Riedel thyroiditis), these are now understood as manifestations of a single systemic disease. IgG4-RD can affect virtually any organ, most commonly pancreas, biliary tree, salivary glands, lacrimal glands, retroperitoneum, kidneys, and aorta. It typically affects middle-aged to elderly men and responds well to glucocorticoids, though relapse is common. Rituximab is increasingly used for steroid-sparing. The main differential is malignancy.
Key Facts
- Definition: Immune-mediated fibroinflammatory condition with IgG4+ plasma cell infiltration
- Incidence: 0.8-1.0 per 100,000; likely underdiagnosed
- Peak Demographics: Middle-aged to elderly (median 60 years); M:F 2-3:1
- Common Organs: Pancreas, biliary, salivary, lacrimal, retroperitoneum, kidney, aorta
- Pathognomonic: Storiform fibrosis + obliterative phlebitis + IgG4+ plasma cells (>40% ratio)
- Gold Standard Investigation: Histopathology with IgG4 immunostaining
- First-line Treatment: Glucocorticoids (prednisone 40mg, taper over 3-6 months)
- Prognosis: Excellent steroid response; 30-50% relapse
Clinical Pearls
Diagnostic Pearl: Serum IgG4 is elevated in only 60-70% - do NOT use as sole diagnostic criterion. Histology is essential.
Treatment Pearl: Response to steroids is typically rapid and dramatic. Lack of response should prompt reconsideration of diagnosis.
Pitfall Warning: IgG4-RD can mimic malignancy (pancreatic, retroperitoneal). Always exclude cancer before diagnosing.
Mnemonic: IgG4 - Inflammation chronically, Giant cells absent, Greater than forty percent ratio, 4 is the subclass
Why This Matters Clinically
IgG4-RD is increasingly recognised and treatable. Its mimicry of malignancy means it enters differential diagnosis of many mass lesions. Early treatment prevents irreversible fibrosis and organ damage.
Incidence
- Estimated 0.8-1.0 per 100,000 per year
- Autoimmune pancreatitis: 0.8 per 100,000
Demographics
| Factor | Details |
|---|---|
| Age | Median 60 years; range 40-80 |
| Sex | M:F 2-3:1 (except head/neck: equal) |
| Ethnicity | Higher recognition in Japan; likely global |
Risk Factors
- No clear risk factors identified
- ? Genetic susceptibility (HLA associations under investigation)
- History of atopy in some patients
Mechanism
Step 1: Immune Trigger (Unknown)
- Unclear initiating event
- ? Molecular mimicry, environmental antigen
- Loss of tolerance to self-antigens
Step 2: Immune Response
- CD4+ T cells (Th2 and Tfh) drive pathology
- Activation of B cells and plasmablasts
- IgG4 class switching (though IgG4 may not be directly pathogenic)
- Cytokines: IL-4, IL-10, IL-13, TGF-β
Step 3: Tissue Infiltration
- Dense lymphoplasmacytic infiltrate
- High proportion of IgG4+ plasma cells (>40% of IgG+ cells)
- Eosinophil infiltration in some cases
Step 4: Fibrosis
- TGF-β and other cytokines drive fibroblast activation
- Storiform (cartwheel/matted) fibrosis pattern
- Obliterative phlebitis (vein occlusion by inflammation)
- Mass-forming lesions ("tumefactive")
Step 5: Organ Dysfunction
- Obstructive phenomena (biliary, ureteric)
- Glandular destruction (salivary, lacrimal)
- Vascular complications (aortitis, aneurysm)
- If untreated: irreversible fibrosis
Histological Criteria (Boston Consensus)
For diagnosis, require:
- Dense lymphoplasmacytic infiltrate
- Storiform fibrosis
- Obliterative phlebitis
Plus: IgG4+ plasma cells >10/HPF and IgG4+:IgG+ ratio >40%
Organ Manifestations
| Organ | Manifestation | Features |
|---|---|---|
| Pancreas | Type 1 AIP | Obstructive jaundice, mass, diabetes |
| Biliary | IgG4-cholangitis | Strictures, mimics cholangiocarcinoma |
| Salivary | IgG4-sialadenitis (Mikulicz) | Bilateral parotid/submandibular swelling |
| Lacrimal | IgG4-dacryoadenitis | Bilateral lacrimal gland enlargement |
| Orbit | IgG4-ophthalmic disease | Proptosis, EOM dysfunction |
| Retroperitoneum | RPF | Ureteric obstruction, hydronephrosis |
| Kidney | Tubulointerstitial nephritis | Renal failure, mass lesion |
| Aorta | IgG4-aortitis | Inflammatory aneurysm, wall thickening |
| Thyroid | Riedel thyroiditis | Woody hard thyroid |
| Lung | IgG4-lung disease | Nodules, interstitial disease |
| Meninges | IgG4-pachymeningitis | Headache, cranial neuropathy |
Presentation Patterns
Red Flags
[!CAUTION]
- Mass suspicious for malignancy - biopsy essential
- Biliary obstruction requiring stenting
- Aortic aneurysm
- Acute renal failure
Assessment
Head/Neck:
- Bilateral salivary gland enlargement
- Lacrimal gland swelling
- Proptosis
- Thyroid: woody hard (Riedel)
Abdominal:
- Jaundice
- Hepatomegaly (if biliary obstruction)
- Flank masses (kidney)
Cardiovascular:
- Aortic aneurysm (palpable if abdominal)
General:
- Usually well-appearing despite significant organ involvement
Laboratory
| Test | Finding | Notes |
|---|---|---|
| Serum IgG4 | Elevated >135 mg/dL | Only 60-70% sensitivity; not specific |
| Total IgG | Often elevated | |
| IgE | May be elevated | Atopic features |
| Eosinophils | May be elevated | Peripheral eosinophilia in 30% |
| Inflammatory markers | ESR, CRP normal or mildly elevated | Typically not highly inflammatory |
| LFTs | Cholestatic pattern if biliary | |
| Creatinine | Elevated if TIN | |
| Complement (C3/C4) | May be low | Immune complex deposition |
Imaging
| Modality | Findings |
|---|---|
| CT/MRI | Organ swelling, mass lesions, capsule-like rim |
| Pancreas CT | "Sausage-shaped" pancreas, delayed enhancement |
| CT urogram | Retroperitoneal fibrosis surrounding aorta, ureters |
| PET-CT | FDG-avid lesions (distinguishes active from fibrotic) |
Histology (Gold Standard)
Obtain biopsy whenever possible
Major criteria:
- Dense lymphoplasmacytic infiltrate
- Storiform fibrosis
- Obliterative phlebitis
Minor: IgG4+ plasma cells >10/HPF, IgG4:IgG ratio >40%
Algorithm
First-Line: Glucocorticoids
| Regimen | Dose | Duration |
|---|---|---|
| Induction | Prednisone 40mg/day (0.6mg/kg) | 2-4 weeks |
| Taper | Reduce by 5mg every 2 weeks | 3-6 months total |
| Maintenance | Consider 5-10mg long-term in relapsers | Variable |
Response: Usually rapid (days-weeks); lack of response should prompt reconsideration
Second-Line: Rituximab
| Indication | Regimen |
|---|---|
| Relapsing disease | Rituximab 1g x2 (2 weeks apart) |
| Steroid intolerance | Rituximab |
| Steroid-sparing | Rituximab maintenance every 6 months |
Other Agents
- Azathioprine, mycophenolate (steroid-sparing but less effective than rituximab)
- No role for cyclophosphamide typically
Organ-Specific Management
| Organ | Intervention |
|---|---|
| Biliary obstruction | ERCP + stent, then steroids |
| Hydronephrosis | Ureteric stent, steroids |
| Aortic aneurysm | Vascular surgery if critical, steroids |
Exclude Malignancy
- Always obtain tissue diagnosis before immunosuppression
- Pancreatic IgG4-RD can closely mimic cancer
| Complication | Management |
|---|---|
| Obstructive jaundice | ERCP, biliary stenting |
| Hydronephrosis/renal failure | Ureteric stent, dialysis if needed |
| Aortic rupture | Vascular surgery |
| Irreversible fibrosis | Permanent organ dysfunction |
| Steroid side effects | Monitor, steroid-sparing |
Outcomes
- Excellent response to steroids (>90%)
- Relapse rate: 30-50%
- Disease progression rare with treatment
- Mortality low (mainly from untreated complications)
Prognostic Factors
Good:
- Early treatment
- Single organ involvement
- Rituximab use for relapsers
Poor:
- Delayed diagnosis with established fibrosis
- Multi-organ involvement
- Aortitis with aneurysm
Key Guidelines
- International Consensus Guidance (2015) — Stone et al. Comprehensive diagnostic and therapeutic recommendations. PMID: 25796218
- ACR/EULAR Classification Criteria (2019) — Validation study for IgG4-RD classification. PMID: 31618526
Key Studies
- Rituximab trials — Multiple observational studies showing efficacy in relapsing disease
What is IgG4-Related Disease?
Your immune system is causing inflammation and scarring in certain organs. This can cause swelling and problems in areas like salivary glands, the pancreas, or around blood vessels.
How is it treated?
Steroid tablets usually work very well. Some people need a medication called rituximab if the disease comes back.
What to watch for
- New swelling
- Jaundice (yellowing skin/eyes)
- Pain or changes in affected areas
-
Stone JH et al. IgG4-Related Disease. N Engl J Med. 2012;366(6):539-551. PMID: 22316447
-
Stone JH et al. Recommendations for the nomenclature of IgG4-related disease. Arthritis Rheumatol. 2015;67(7):1688-1699. PMID: 25796218
-
Wallace ZS et al. ACR/EULAR IgG4-RD Classification Criteria. Ann Rheum Dis. 2020;79(1):77-87. PMID: 31618526
-
Carruthers MN et al. Rituximab for IgG4-related disease. Ann Rheum Dis. 2015;74(6):1171-1177. PMID: 24442885
-
Deshpande V et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25(9):1181-1192. PMID: 22596100
Viva Points
"IgG4-RD is a fibroinflammatory condition with tumefactive lesions, dense lymphoplasmacytic infiltrate with IgG4+ plasma cells, and storiform fibrosis. Commonly affects pancreas, biliary, salivary, lacrimal, retroperitoneum. Responds well to steroids; rituximab for relapse."
Key Facts
- Histology is gold standard, not serum IgG4
- IgG4+ plasma cells >40% ratio
- Exclude malignancy before treating
- Response to steroids is rapid
- Relapse common (30-50%)
Common Mistakes
- ❌ Diagnosing on high serum IgG4 alone
- ❌ Starting steroids without biopsy (may miss cancer)
- ❌ Not considering IgG4-RD in unexplained pancreatitis or RPF
Last Reviewed: 2026-01-01 | MedVellum Editorial Team