Minimal Change Disease
Summary
Minimal change disease (MCD) is the most common cause of nephrotic syndrome in children (80%) and accounts for 10-25% of adult nephrotic syndrome. It is characterised by heavy proteinuria, hypoalbuminaemia, and oedema, with a renal biopsy showing normal glomeruli on light microscopy but diffuse podocyte foot process effacement on electron microscopy. The pathogenesis involves T-cell dysfunction and circulating permeability factors affecting the glomerular filtration barrier. MCD is highly steroid-responsive - 90% of children and 80-90% of adults achieve remission with corticosteroids. However, relapses are common (50-70%), and a subset become steroid-dependent or steroid-resistant, requiring second-line immunosuppression.
Key Facts
- Definition: Glomerular disease with nephrotic syndrome, normal LM, and podocyte foot process effacement on EM
- Incidence: Children 2-7 per 100,000; Adults 0.5-1 per 100,000
- Peak Demographics: Children 2-6 years; Adults bimodal (20-30 and >65)
- Pathognomonic Feature: Heavy proteinuria with normal light microscopy; foot process effacement on EM
- Gold Standard Investigation: Renal biopsy (adults); often empirical treatment in children
- First-line Treatment: Prednisolone 1mg/kg/day (max 80mg) for 4-16 weeks
- Prognosis: 90% steroid-responsive; excellent long-term renal prognosis
Clinical Pearls
Diagnostic Pearl: In children with typical nephrotic syndrome presentation (2-6 years, no haematuria, no hypertension, normal complement), empirical steroids without biopsy is standard - biopsy if atypical features or steroid resistance.
Treatment Pearl: Adults require longer steroid courses than children (16 weeks vs 8-12 weeks) for optimal response.
Pitfall Warning: Nephrotic syndrome is a hypercoagulable state - prophylactic anticoagulation may be needed if albumin less than 20 g/L or high risk factors.
Mnemonic: MCD - Minimal on light microscopy, Complete response to steroids, Diffuse foot process effacement
Why This Matters Clinically
MCD is the paradigm of steroid-responsive nephrotic syndrome. Understanding its management informs approach to all glomerular diseases. Complications of nephrotic syndrome (thromboembolism, infection) require proactive prevention.
Incidence
- Children: 2-7 per 100,000 per year (80% of childhood nephrotic syndrome)
- Adults: 0.5-1 per 100,000 per year (10-25% of adult nephrotic syndrome)
Demographics
| Factor | Details |
|---|---|
| Age | Children 2-6 years; Adults bimodal 20-30 and >65 |
| Sex | Children M:F 2:1; Adults M:F 1:1 |
| Ethnicity | More common in South Asians |
Risk Factors/Associations
| Association | Notes |
|---|---|
| Atopy | Strong association with allergies, asthma, eczema |
| NSAIDs | Drug-induced MCD |
| Lithium | Drug-induced |
| Hodgkin lymphoma | Secondary MCD |
| Thymoma | Paraneoplastic |
| Viral infections | May trigger relapse |
Mechanism
Step 1: T-cell Dysfunction
- Abnormal T-cell activation (especially CD4+ and Tregs)
- Production of circulating permeability factors (CPF) - exact identity unknown
- Associated with atopy, allergic disorders
Step 2: Podocyte Injury
- CPF targets podocytes (glomerular epithelial cells)
- Loss of podocyte negative charge and slit diaphragm integrity
- Foot process effacement (flattening and fusion)
Step 3: Loss of Glomerular Barrier
- Normal glomerular filtration barrier has charge and size selectivity
- Loss of charge selectivity allows albumin (negatively charged) to pass
- Massive proteinuria (>3.5g/day in adults)
Step 4: Nephrotic Syndrome Development
- Heavy proteinuria → hypoalbuminaemia
- Reduced oncotic pressure → oedema
- Hyperlipidaemia (hepatic lipid synthesis increased)
- Hypercoagulability (loss of anticoagulant proteins, increased clotting factors)
Step 5: Resolution with Treatment
- Corticosteroids suppress T-cell function and CPF production
- Podocyte recovery with regeneration of foot processes
- Resolution of proteinuria (remission)
Histopathology
| Modality | Findings |
|---|---|
| Light Microscopy | Normal (hence "minimal change") |
| Immunofluorescence | Negative or trace IgM, C3 |
| Electron Microscopy | Diffuse podocyte foot process effacement (pathognomonic) |
Symptoms
Signs
Red Flags
[!CAUTION]
- Signs of thromboembolism (leg swelling, dyspnoea - PE)
- Fever/abdominal pain (spontaneous bacterial peritonitis)
- Severe hypoalbuminaemia less than 20 g/L
- AKI (may occur in severe cases)
Assessment
General:
- Oedema assessment: periorbital, peripheral, sacral
- Daily weights
Cardiovascular:
- Blood pressure (usually normal in MCD)
- Volume status
Abdominal:
- Ascites (shifting dullness)
- Umbilical/scrotal oedema
Respiratory:
- Pleural effusions (reduced breath sounds)
Laboratory
| Test | Finding | Purpose |
|---|---|---|
| Urinalysis | Proteinuria 3-4+, no haematuria | Initial screen |
| Urine PCR/ACR | >300 mg/mmol (nephrotic range) | Quantify proteinuria |
| 24h urine protein | >3.5g/day | Nephrotic diagnosis |
| Serum albumin | less than 25 g/L (often less than 20) | Severity |
| Lipid profile | Elevated cholesterol, LDL | Nephrotic syndrome |
| U&E | Usually normal; AKI possible | Renal function |
| Complement (C3/C4) | Normal | Exclude other GN |
| Serum/urine electrophoresis | Exclude myeloma | Adults >40 |
| Hepatitis B/C, HIV | Exclude secondary causes | All adults |
Imaging
| Modality | Indication |
|---|---|
| Renal ultrasound | Normal or enlarged kidneys; exclude other pathology |
| Doppler | If renal vein thrombosis suspected |
Renal Biopsy
Indications in children:
- Atypical features (haematuria, hypertension, renal impairment)
- Age less than 1 year or >12 years
- Steroid resistance
Indication in adults:
- Always required (to differentiate from FSGS, membranous, etc.)
Algorithm
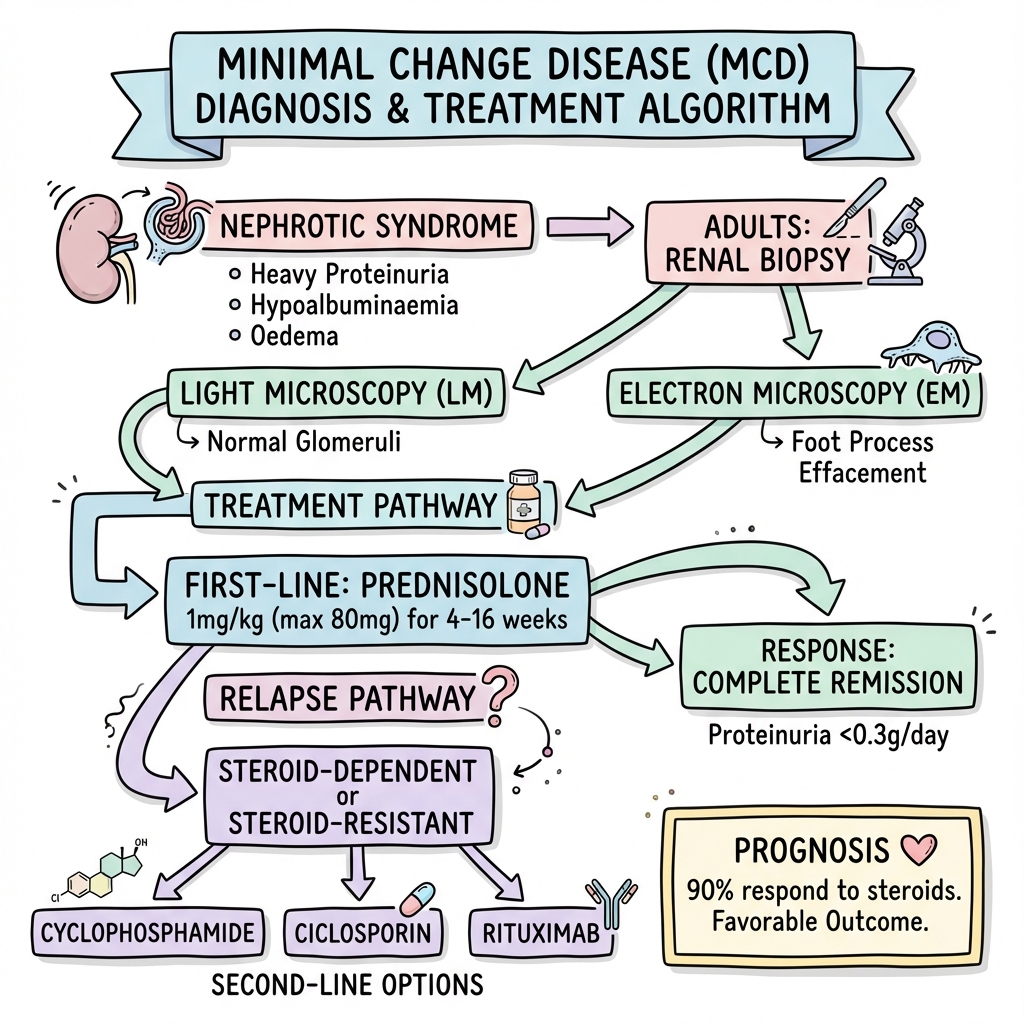
First-Line: Corticosteroids
Adults:
- Prednisolone 1mg/kg/day (max 80mg) for 4 weeks minimum
- Then taper over 12-16 weeks total
- Response may take longer than children (4-16 weeks)
Children (empirical treatment):
- Prednisolone 60mg/m²/day (max 60mg) for 4 weeks
- Then 40mg/m² alternate days for 4 weeks
- Taper
Definitions
| Response | Definition |
|---|---|
| Complete remission | Proteinuria less than 0.3g/day or uPCR less than 30 |
| Partial remission | >50% reduction but still nephrotic |
| Steroid resistance | Failure to remit after 16 weeks (adults) or 4-8 weeks (children) |
| Relapse | Recurrence of proteinuria >3g/day or uPCR >200 |
| Frequent relapser | ≥2 relapses in 6 months or ≥4 in 12 months |
| Steroid dependent | Relapse on weaning or within 2 weeks of stopping steroids |
Second-Line Therapy
| Indication | Options |
|---|---|
| Steroid-dependent | Cyclophosphamide 2mg/kg for 8-12 weeks (once only) |
| Ciclosporin/Tacrolimus | |
| Rituximab (increasingly used) | |
| Mycophenolate mofetil | |
| Steroid-resistant | Calcineurin inhibitor (ciclosporin/tacrolimus) |
| Add low-dose steroids | |
| Rituximab | |
| Re-biopsy to confirm diagnosis/exclude FSGS | |
| Frequent relapsing | As per steroid-dependent |
Supportive Care
Oedema:
- Salt restriction (less than 2g/day sodium)
- Fluid restriction if severe
- Loop diuretics (furosemide ± thiazide)
- Albumin infusion if severe hypoalbuminaemia with diuretics
Thromboprophylaxis:
- Consider prophylactic anticoagulation if albumin less than 20 g/L
- Encourage mobility
Infection Prevention:
- Low threshold for antibiotics
- Consider pneumococcal vaccination
Hyperlipidaemia:
- Usually resolves with remission
- Statins if persistent
Disposition
- Admit: Severe oedema, complications (infection, AKI, VTE), initiation of therapy
- Outpatient: Mild cases, follow-up monitoring
- Nephrology follow-up: Essential for monitoring relapses, steroid side effects
Complications of Nephrotic Syndrome
| Complication | Incidence | Management |
|---|---|---|
| Thromboembolism (DVT, PE, RVT) | 5-25% | Anticoagulation, prevention |
| Infection (SBP, cellulitis, pneumonia) | Common | Low threshold antibiotics |
| AKI | 5-10% | Volume management, avoid nephrotoxins |
| Hyperlipidaemia | Universal | Statins if persistent |
| Protein malnutrition | If prolonged | Nutritional support |
Treatment-Related
- Steroid side effects: Weight gain, diabetes, osteoporosis, infection
- Cyclophosphamide: Bone marrow suppression, gonadal toxicity
- Ciclosporin: Nephrotoxicity, hypertension
Outcomes
| Population | Steroid Response | Long-term Prognosis |
|---|---|---|
| Children | 90-95% complete remission | Excellent; rare ESKD |
| Adults | 80-90% complete remission | Good; higher relapse than children |
- Relapse rate: 50-70% (higher in children)
- ESKD: less than 5% (mainly steroid-resistant cases, which often are FSGS on re-biopsy)
Prognostic Factors
Good:
- Rapid steroid response
- Complete remission
- Childhood onset
Poor:
- Steroid resistance (may indicate FSGS)
- Adult onset
- Frequent relapses
- Development of steroid complications
Key Guidelines
- KDIGO Glomerulonephritis Guidelines (2021) — Updated guidance on GN including MCD PMID: 34556300
- Renal Association UK Clinical Practice Guidelines — MCD management
Key Evidence
- MCD treatment largely based on observational data and RCTs for prevention of relapse
- PREDNOS Trial — Evaluated steroid regimens in childhood nephrotic syndrome
- Rituximab — Increasing evidence for steroid-dependent disease PMID: 29626047
What is Minimal Change Disease?
Your kidneys have tiny filters. In MCD, there's a problem with the filter barrier that lets protein leak into your urine. Under the microscope, the filters look almost normal (hence "minimal change"), but special microscopy shows tiny changes.
How is it treated?
Most people respond very well to steroids (prednisolone). Treatment lasts several months. Some people relapse (it comes back) and need further treatment.
What to watch for
- Leg or face swelling getting worse
- Breathlessness
- Fever or infection
- Blood clots (pain/swelling in leg)
-
KDIGO Glomerulonephritis Work Group. KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Kidney Int. 2021;100(4S):S1-S276. PMID: 34556300
-
Vivarelli M et al. Minimal Change Disease. Clin J Am Soc Nephrol. 2017;12(2):332-345. PMID: 27940460
-
Ruggenenti P et al. Rituximab in Steroid-Dependent or Frequently Relapsing Idiopathic Nephrotic Syndrome. J Am Soc Nephrol. 2014;25(4):850-863. PMID: 24480825
-
Maas RJ et al. Minimal change disease and idiopathic FSGS: manifestations of the same disease. Nat Rev Nephrol. 2016;12(8):445-454. PMID: 27297766
-
Lombel RM et al. Treatment of Steroid-Sensitive Nephrotic Syndrome: New Guidelines from KDIGO. Pediatr Nephrol. 2013;28(3):415-426. PMID: 23052049
Viva Points
"Minimal change disease is the most common cause of nephrotic syndrome in children (80%). It shows normal light microscopy with foot process effacement on electron microscopy. 90% respond to corticosteroids. Relapses are common (50-70%). Steroid-sparing agents include cyclophosphamide, ciclosporin, and rituximab."
Key Facts
- Normal LM, foot process effacement EM
- Nephrotic syndrome without haematuria/hypertension
- 90% steroid-responsive
- Biopsy in adults; empirical steroids in children
Common Mistakes
- ❌ Not recognising hypercoagulable state
- ❌ Biopsying typical childhood nephrotic syndrome
- ❌ Too short steroid courses in adults
- ❌ Missing secondary causes (NSAIDs, lymphoma)
Last Reviewed: 2026-01-01 | MedVellum Editorial Team