Sarcoidosis
Summary
Sarcoidosis is a multisystem granulomatous disease of unknown aetiology characterised by non-caseating granulomas. It most commonly affects the lungs and intrathoracic lymph nodes but can involve virtually any organ including skin, eyes, heart, and nervous system. The disease predominantly affects young adults (20-40 years) and has higher prevalence in African Americans and Scandinavians. Diagnosis is based on compatible clinical and radiological features with histological confirmation of non-caseating granulomas after exclusion of other causes (especially TB). Many patients are asymptomatic and require observation only. Treatment with corticosteroids is reserved for symptomatic or organ-threatening disease.
Key Facts
- Definition: Multisystem granulomatous disease with non-caseating granulomas
- Incidence: 10-40 per 100,000; higher in African Americans
- Peak Demographics: 20-40 years; slight female predominance
- Pathognomonic: Non-caseating granulomas (must exclude TB)
- Classification: CXR staging (I-IV)
- Gold Standard Investigation: Tissue biopsy showing non-caseating granulomas
- First-line Treatment: Observation if mild; corticosteroids if symptomatic
- Prognosis: 60-70% remit spontaneously; 10-30% chronic
Clinical Pearls
Diagnostic Pearl: Lofgren syndrome (erythema nodosum + bilateral hilar lymphadenopathy + polyarthritis + fever) is pathognomonic - biopsy often not needed.
Treatment Pearl: Stage I sarcoidosis usually spontaneously remits - observe, do not treat unless symptomatic.
Pitfall Warning: Always exclude TB before diagnosing sarcoidosis - granulomas look similar but TB granulomas are caseating.
Why This Matters Clinically
Sarcoidosis is common and often discovered incidentally. Knowing when to treat and when to observe prevents overtreatment. Screening for cardiac and neurological involvement prevents serious complications.
Incidence
- 10-40 per 100,000 per year (varies by population)
- African Americans: 35-80 per 100,000 (higher, more severe)
- Scandinavians: Higher incidence
Demographics
- Age: 20-40 years (bimodal with second peak in women over 50)
- Sex: Slight female predominance
- Ethnicity: Higher in African Americans, Scandinavians
Mechanism
Step 1: Unknown Trigger
- Environmental antigen, infectious agent, or autoimmune process
- Genetic susceptibility (HLA associations)
Step 2: Th1 Immune Response
- CD4+ T helper 1 cells activated
- Macrophage activation via IFN-gamma, TNF-alpha
Step 3: Granuloma Formation
- Non-caseating epithelioid granulomas
- Giant cells (Langhans and foreign body type)
- Surrounded by lymphocytes
Step 4: Organ Involvement
- Lungs and lymph nodes most common
- Can affect any organ
- Some granulomas resolve; others cause fibrosis
Pulmonary (90%)
Extrapulmonary
| Organ | Manifestation |
|---|---|
| Skin | Erythema nodosum, lupus pernio, plaques |
| Eyes | Uveitis (anterior most common), lacrimal gland |
| Heart | Arrhythmias, heart block, cardiomyopathy |
| Neurological | CN palsies (VII most common), meningitis, seizures |
| Joints | Polyarthritis |
| Liver/spleen | Hepatomegaly, elevated ALP |
| Kidney | Hypercalcaemia, nephrocalcinosis |
Lofgren Syndrome (Acute Sarcoidosis)
Heerfordt Syndrome
Red Flags
[!CAUTION]
- Syncope, palpitations (cardiac)
- Neurological symptoms
- Hypercalcaemia
- Progressive dyspnoea despite treatment
CXR Staging
| Stage | Findings | Spontaneous Remission |
|---|---|---|
| 0 | Normal | N/A |
| I | BHL only | 60-90% |
| II | BHL + parenchymal infiltrates | 40-70% |
| III | Parenchymal infiltrates, no BHL | 10-20% |
| IV | Pulmonary fibrosis | 0% |
Laboratory
| Test | Finding |
|---|---|
| ACE | Elevated (60-70%) - not specific |
| Calcium | Hypercalcaemia (10%) from 1,25-OH vitamin D |
| LFTs | Elevated ALP if hepatic |
| sIL-2R | Elevated (marker of activity) |
Imaging
- CXR: BHL, parenchymal infiltrates, fibrosis
- HRCT: Perilymphatic nodules, fibrosis
- PET: May show active disease
Biopsy
- Bronchoscopy with transbronchial biopsy (TBB) or EBUS-TBNA
- Lymph node biopsy
- Skin biopsy if lesions present
Screening for Extrapulmonary
- Eyes: Ophthalmology review
- Heart: ECG, echo, consider CMR or PET
- Baseline U and E, calcium, LFTs
Algorithm
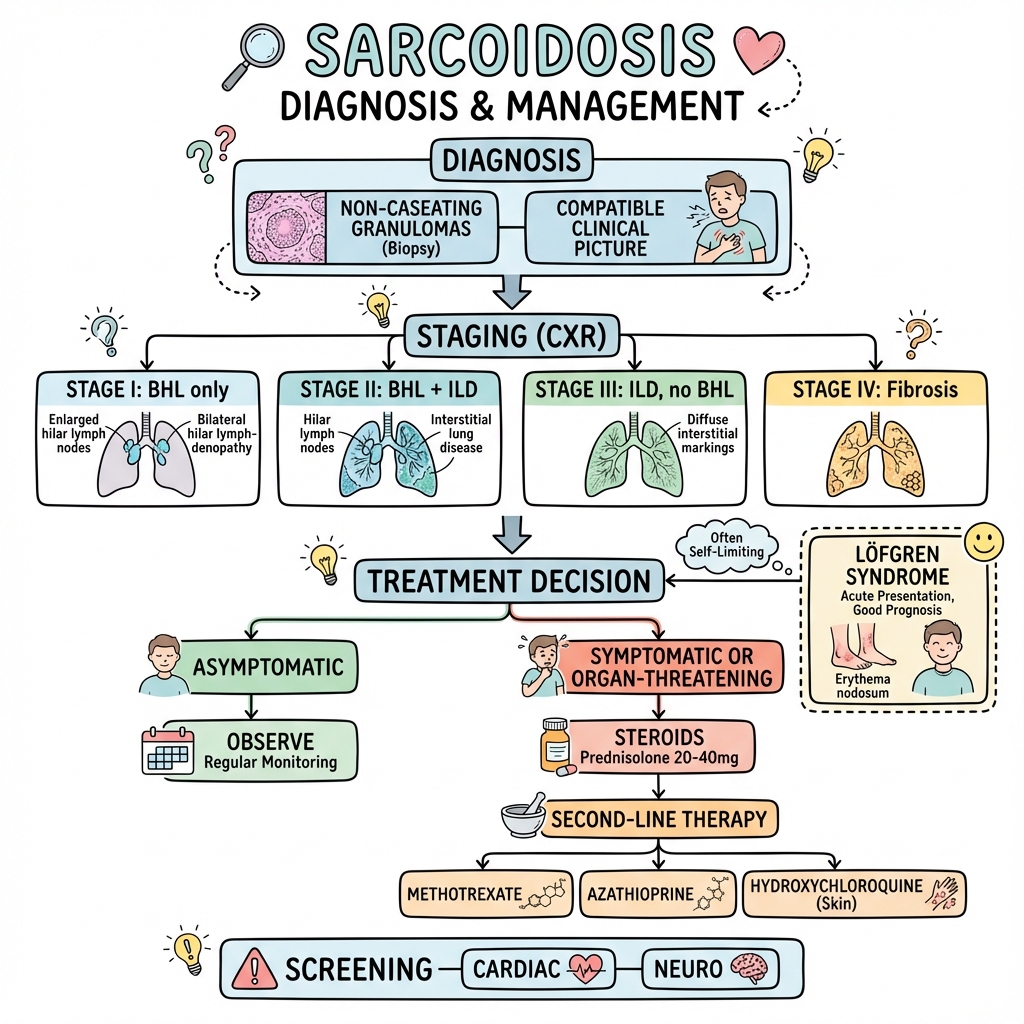
Observation
- Asymptomatic Stage I or mild Stage II
- Monitor PFTs, CXR
Corticosteroids
| Indication | Dose |
|---|---|
| Symptomatic pulmonary | Prednisolone 20-40mg daily, taper over 6-12 months |
| Cardiac/neurological | Higher doses; specialist input |
| Hypercalcaemia | Steroids usually effective |
Steroid-Sparing Agents
| Agent | Use |
|---|---|
| Methotrexate | Most commonly used |
| Azathioprine | Alternative |
| Mycophenolate | Alternative |
| Hydroxychloroquine | Skin, hypercalcaemia |
| TNF inhibitors | Refractory disease |
Specific Organ Treatment
- Cardiac: Steroids, consider ICD
- Neurosarcoidosis: High-dose steroids, biologics
- Eye: Topical steroids; systemic if severe
Outcomes
- Spontaneous remission: 60-70%
- Chronic course: 10-30%
- Mortality: less than 5% (cardiac, pulmonary fibrosis)
-
Statement on Sarcoidosis. Am J Respir Crit Care Med. 1999;160(2):736-755. PMID: 10430755
-
Baughman RP et al. Treatment of sarcoidosis. Clin Chest Med. 2015;36(4):751-767. PMID: 26593147
-
Iannuzzi MC et al. Sarcoidosis. N Engl J Med. 2007;357(21):2153-2165. PMID: 18032765
Viva Points
"Sarcoidosis is a multisystem granulomatous disease with non-caseating granulomas. Lungs most commonly affected. Stage I often remits spontaneously. Treat with steroids if symptomatic. Screen for cardiac and neuro involvement."
Key Facts
- Non-caseating granulomas (exclude TB)
- Lofgren syndrome = excellent prognosis
- Elevated ACE (not specific)
- Stage I often resolves spontaneously
Common Mistakes
- Treating asymptomatic Stage I
- Not screening for cardiac/neuro involvement
- Missing hypercalcaemia
Last Reviewed: 2026-01-01 | MedVellum Editorial Team