Infective Endocarditis
Summary
Infective endocarditis (IE) is a microbial infection of the endocardial surface of the heart, predominantly affecting cardiac valves. Despite advances in diagnosis and treatment, IE remains life-threatening with in-hospital mortality of 15-30% and 1-year mortality approaching 40%. The epidemiology has shifted: previously dominated by rheumatic heart disease in young patients, IE now affects older patients with degenerative valves, those with prosthetic valves, and intravenous drug users. The Modified Duke Criteria remain the diagnostic cornerstone, combining microbiological evidence with echocardiographic findings. Early surgical consultation is essential, as up to 50% require valve surgery. Recognition requires high clinical suspicion, as presentations can be insidious and classical signs may be absent.
Key Facts
- Definition: Infection of endocardial surface with vegetation formation (platelets, fibrin, microorganisms, inflammatory cells)
- Incidence: 3-10 per 100,000 person-years; rising with aging population
- Mortality: In-hospital 15-30%; 1-year mortality 30-40%
- Morbidity: Embolic events 20-50%, heart failure 30-40%, perivalvular abscess 10-40%
- Peak Demographics: Bimodal - IVDU (20-40 years) and elderly degenerative (>65 years); Male:Female 2:1
- Pathognomonic Feature: Vegetation on echo with positive blood cultures for typical organisms
- Gold Standard Investigation: TEE - sensitivity 90-100% vs TTE 50-60%
- First-line Treatment: Empirical IV antibiotics + surgical evaluation
- Prognosis: With treatment 70% survive to 1 year; without surgery when indicated mortality exceeds 50%
Clinical Pearls
Diagnostic Pearl: Three blood culture sets from different venepuncture sites before antibiotics identify causative organism in >90%. Never give antibiotics before cultures in stable patients.
Examination Pearl: Splinter haemorrhages, Janeway lesions, and Osler nodes present in only 10-25%. New or changing murmur is the most important clinical sign.
Treatment Pearl: Prosthetic valve IE requires rifampicin to penetrate biofilm, but only after 3-5 days bactericidal therapy to prevent resistance.
Pitfall Warning: Negative cultures occur in 10-20% - consider prior antibiotics, fastidious organisms (HACEK, Coxiella, Bartonella), or fungal infection.
Mnemonic: FROM JANE - Fever, Roth spots, Osler nodes, Murmur (new), Janeway, Anaemia, Nail haemorrhages, Emboli
Why This Matters Clinically
Infective endocarditis is a great mimicker - missed or delayed diagnosis leads to catastrophic outcomes including stroke and death. Medico-legal cases frequently arise from failure to obtain blood cultures before antibiotics, inadequate echo assessment, and delayed surgical referral. Core topic for MRCP Part 2 and FRCS viva examinations. Healthcare-associated IE is increasing, making this relevant across all hospital specialties.
Incidence and Prevalence
- Incidence: 3-10 per 100,000 person-years globally; up to 15 per 100,000 in elderly
- Prevalence: Point prevalence ~1 per 10,000 hospitalized patients
- Lifetime Risk: 0.5-1% general population; 2-5% with predisposing valve lesions
- Trend: Increasing over 20 years due to aging, prosthetic devices, healthcare-associated infections
- Geographic Variation: Higher in developed countries; lower where rheumatic fever declining
- Temporal Trends: No seasonal variation; healthcare-associated now 25-30%
Demographics
| Factor | Details | Clinical Significance |
|---|---|---|
| Age | Peak: 70-80y; secondary 25-40 (IVDU) | Elderly have higher mortality |
| Sex | Male:Female 2:1 | Higher valve disease in men |
| Ethnicity | Higher Indigenous (Aus/NZ) | RHD prevalence |
| Geography | Higher urban areas | IVDU populations |
| Socioeconomic | Strong disadvantage association | IVDU, delayed presentation |
| Occupation | Healthcare workers minor risk | Needle-stick, MRSA |
Risk Factors
Non-Modifiable:
| Factor | Relative Risk (95% CI) | Mechanism |
|---|---|---|
| Prior endocarditis | RR 8.0 (5.2-12.3) | Damaged endothelium |
| Prosthetic valve | RR 5.0-20.0 | Foreign body, biofilm |
| Congenital heart disease | RR 4.0-8.0 | Abnormal flow |
| Rheumatic heart disease | RR 3.0-5.0 | Valve scarring |
| Degenerative valve disease | RR 2.0-4.0 | Endothelial disruption |
| Male sex | RR 1.5-2.0 | Unknown mechanism |
Modifiable:
| Factor | Relative Risk | Evidence | Intervention Impact |
|---|---|---|---|
| IVDU | RR 20-50 | Level 2a | Harm reduction reduces 60-70% |
| Poor dental hygiene | RR 1.5-2.5 | Level 2b | Regular dental care |
| Haemodialysis | RR 3.0-5.0 | Level 2a | Catheter care protocols |
| Central venous catheter | RR 4.0-8.0 | Level 1b | Insertion bundles |
| Diabetes mellitus | RR 2.0-3.0 | Level 2a | Glycaemic control |
| Immunosuppression | RR 2.0-4.0 | Level 2b | Minimise where possible |
Mechanism
Step 1: Endothelial Damage (Predisposition)
- Normal endothelium resists colonisation
- Endothelial injury (turbulent flow, degenerative changes) exposes subendothelial matrix
- Exposed collagen triggers platelet and fibrin deposition
- Forms non-bacterial thrombotic endocarditis (NBTE) - sterile vegetation
- High-velocity jets create low pressure predisposing areas
Step 2: Bacteraemia and Colonisation (Hours-Days)
- Transient bacteraemia from dental procedures, skin breaks
- S. aureus adheres directly; Strep viridans requires damaged endothelium
- Bacteria bind via adhesins (fibronectin-binding proteins)
- Organisms trigger fibrin/platelet deposition, embedded in vegetation
- Immune evasion: protected from phagocytes within vegetation
- IL-1, IL-6, TNF-α release initiates systemic inflammation
Step 3: Vegetation Growth and Destruction
- Vegetations grow 5-20mm, containing 10^9-10^11 bacteria/gram
- Bacterial proteases cause enzymatic valve destruction
- Cusp perforation → acute regurgitation
- Annular extension → abscess (especially aortic, S. aureus)
- Conduction system involvement → heart block
Step 4: Embolic and Immunological Complications
- Vegetation fragments embolise systemically (left-sided) or pulmonary (right-sided)
- Cerebral emboli: stroke 20-40% before diagnosis
- Splenic infarction: 40% at autopsy
- Mycotic aneurysm from septic emboli
- Immune complex: glomerulonephritis, Osler nodes, Roth spots
- Splenomegaly, anaemia of chronic disease
Step 5: Heart Failure and Death Without Treatment
- Progressive valve destruction → acute regurgitation → HF
- Myocardial abscess may rupture (fistulae, pericarditis)
- Untreated mortality approaches 100%
- Surgery-indicated but not performed: 50% mortality
Classification
Modified Duke Criteria (2023 ESC):
| Category | Criteria Required |
|---|---|
| Definite IE | 2 major, OR 1 major + 3 minor, OR 5 minor |
| Possible IE | 1 major + 1-2 minor, OR 3-4 minor |
| Rejected | Alternative diagnosis, OR resolution ≤4 days antibiotics |
Major Criteria:
- Blood cultures positive for typical organisms from 2 separate cultures
- Positive echo (vegetation, abscess, new prosthetic dehiscence) OR new regurgitation
Minor Criteria:
- Predisposing condition or IVDU
- Fever ≥38°C
- Vascular phenomena (emboli, Janeway lesions)
- Immunological (GN, Osler nodes, Roth spots, positive RF)
- Microbiological evidence not meeting major
By Valve Type:
| Type | Definition | Features |
|---|---|---|
| Native valve | Natural valve | 60-70%, viridans strep common |
| Prosthetic early | less than 1 year post-surgery | CoNS, S. aureus; high mortality |
| Prosthetic late | >1 year post-surgery | Similar to NVE |
| Right-sided | Tricuspid/pulmonary | IVDU, pacemaker; pulmonary emboli |
| Device-related | Pacemaker/ICD | Requires extraction |
Anatomical Considerations
Valve Involvement:
- Mitral: 40-45% (most in RHD)
- Aortic: 30-35% (most IVDU left-sided)
- Tricuspid: 10-15% (80% IVDU IE)
- Pulmonary: less than 5%
- Multiple: 10-20%
Symptoms
Typical:
Atypical:
Signs
Cardiac:
Peripheral/Embolic:
Neurological:
Red Flags
[!CAUTION]
- New murmur with fever
- Acute heart failure with sepsis
- Stroke in young patient with fever
- Multiple embolic events
- New heart block (abscess)
- Prosthetic valve with fever
- IVDU with fever and pleuritic pain
Structured Approach
General:
- Unwell, pale, febrile
- Cachexia, clubbing (late)
- Hands: splinter haemorrhages, Osler nodes
- Palms/soles: Janeway lesions
Cardiovascular:
- Pulse character, BP (wide in AR)
- JVP (RV failure)
- Apex displacement
- Auscultate for new/changed murmur
- Regurgitant murmurs: pansystolic (MR/TR), early diastolic (AR)
Peripheral:
- Eyes: Roth spots, conjunctival petechiae
- Mouth: palatal petechiae, dental caries
- Abdomen: splenomegaly
- Skin: petechiae, track marks
- Neuro: focal deficits
Special Tests
| Test | Technique | Finding | Sens/Spec |
|---|---|---|---|
| Nail bed exam | Inspect proximal | Splinter haemorrhages | 5-15%/80% |
| Finger pad palpation | Gentle pressure | Osler nodes - painful | 10-25%/95% |
| Palm/sole inspection | Visual | Janeway - painless red | 5-10%/95% |
| Fundoscopy | Dilated | Roth spots - flame + pale centre | 2-5%/99% |
| Dynamic auscultation | Valsalva, squat | Murmur intensity change | Variable |
First-Line
- ECG: New PR prolongation (abscess), ischaemia (emboli)
- Urinalysis: Microscopic haematuria (70%), proteinuria
- Observations: Temperature chart, heart failure monitoring
Laboratory
| Test | Finding | Purpose |
|---|---|---|
| Blood cultures x3 | Positive 85-90% | Essential - before antibiotics |
| FBC | Anaemia, leucocytosis | Disease activity |
| CRP/ESR | Markedly elevated | Monitoring response |
| U&E | AKI possible | Renal monitoring |
| LFTs | May be deranged | Embolic complications |
| Complement C3/C4 | Low in GN | Immune complex GN |
| Rheumatoid factor | Positive 50% | Minor Duke criterion |
| Serology | Coxiella, Bartonella | Culture-negative workup |
Imaging
| Modality | Findings | Indication |
|---|---|---|
| TTE | Vegetation, regurgitation | First-line, sens 50-60% |
| TEE | Superior visualisation | Prosthetic, negative TTE, abscess |
| CT Head | Stroke, haemorrhage | Neurological symptoms |
| CT Chest | Septic pulmonary emboli | Right-sided, respiratory symptoms |
| CT Abdomen | Splenic/renal infarct | Abdominal pain, persistent fever |
| PET-CT | Increased valve uptake | Prosthetic IE confirmation |
Diagnostic Criteria
Apply Modified Duke Criteria:
- Suspicion → Blood cultures x3 + TTE
- TTE negative, high suspicion → TEE
- Apply Duke criteria
- "Possible" → Repeat cultures, echo, further imaging
- Culture-negative at 5 days → Serological workup
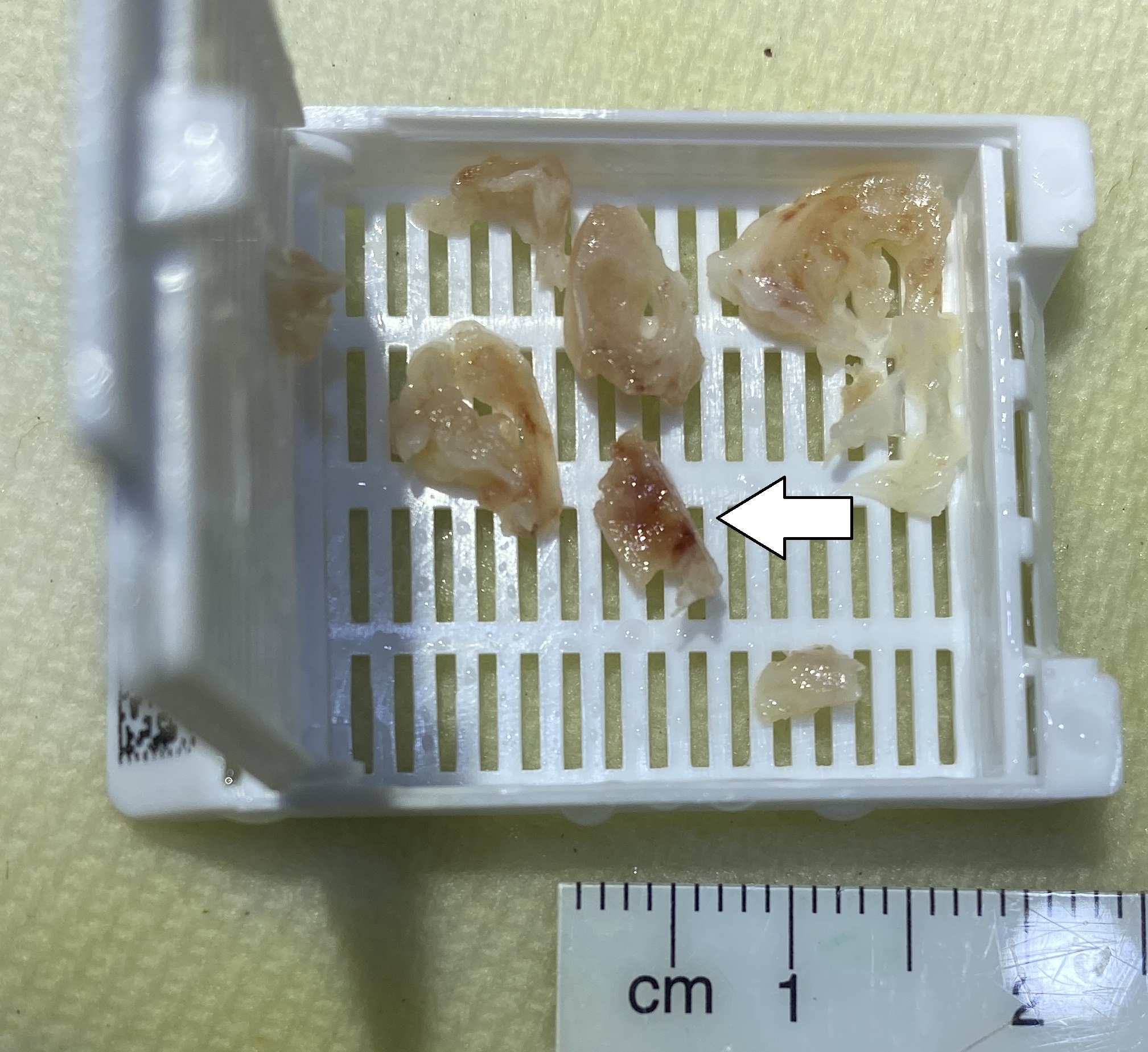
Figure: Gross pathology showing vegetation on mitral valve. Source: Wikipedia Commons (CC0)
Management Algorithm
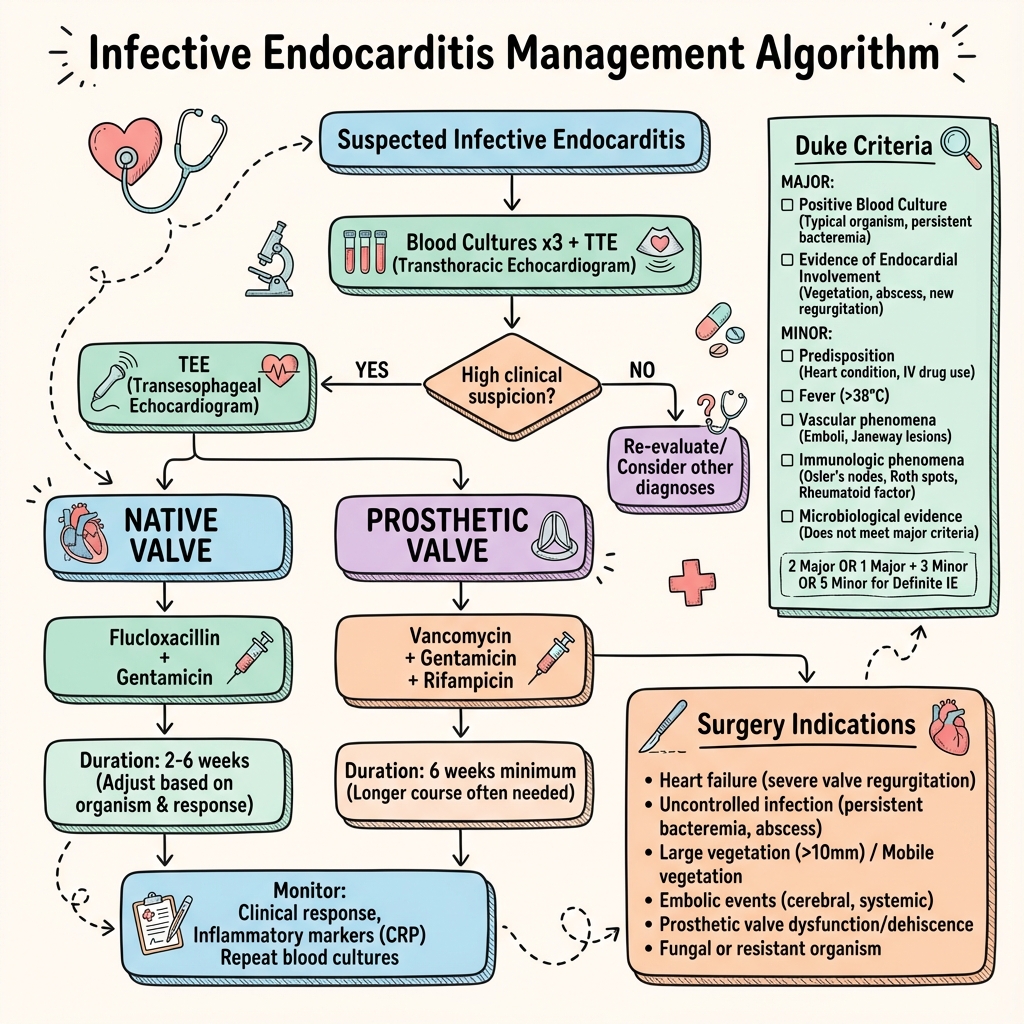
AI-generated algorithm showing workup, empirical antibiotics by valve type, and surgical indications.
Acute/Emergency Management
- Haemodynamic stabilisation - fluids, vasopressors if shock
- Blood cultures x3 before antibiotics (unless unstable)
- Urgent echo - TEE if prosthetic
- Early surgical consultation if high-risk
- Notify microbiology/ID
Conservative Management
- Bed rest acute phase
- DVT prophylaxis
- Nutritional support
- Daily embolic assessment
- Monitor for heart failure
Medical Management
Empirical (Before Culture Results):
| Scenario | Regimen | Duration |
|---|---|---|
| NVE community | Amoxicillin 2g IV 4h + Flucloxacillin 2g IV 4h + Gent 1mg/kg 8h | 4-6 weeks |
| NVE MRSA risk | Vancomycin 15-20mg/kg 12h + Gent 1mg/kg 8h | 4-6 weeks |
| Prosthetic | Vancomycin + Gent + Rifampicin 300mg 12h | 6+ weeks |
| Right-sided IVDU | Flucloxacillin 2g 4h ± Gent | 2-4 weeks |
Targeted (Once Organism Known):
| Organism | First-Line | Duration |
|---|---|---|
| Viridans strep (pen sens) | Benzylpenicillin 1.2g IV 4h | 4 weeks |
| Enterococcus | Amoxicillin 2g 4h + Gent | 4-6 weeks |
| MSSA | Flucloxacillin 2g 4h | 4-6 weeks |
| MRSA | Vancomycin ± Rifampicin | 6 weeks |
| HACEK | Ceftriaxone 2g daily | 4 weeks |
Monitoring:
- Gentamicin levels: pre less than 1, post 3-5 mg/L
- Vancomycin trough: 15-20 mg/L
- Renal function: twice weekly with aminoglycosides
- CRP: should decline by day 7
Surgical Management
Class I Indications (ESC/AHA):
- Heart failure from valve dysfunction
- Uncontrolled infection (fever >7 days, abscess, enlarging vegetation)
- Prevention of embolism (vegetation >10mm after embolus, isolated >15mm)
Timing:
- Emergency (24h): Refractory pulmonary oedema, cardiogenic shock
- Urgent (days): Uncontrolled infection, high embolic risk
- Elective (1-2 weeks): After stabilisation if indication present
Procedures:
- Valve repair (preferred) > replacement
- Abscess debridement
- Mechanical vs bioprosthetic individualised
Disposition
- Admit: All confirmed/suspected IE
- ICU: Septic shock, HF, post-op, stroke
- Discharge: After IV antibiotics complete, stable, no surgery needed
- Follow-up: Cardiology 4 weeks, 3 months, 12 months; echo before discharge
Immediate
| Complication | Incidence | Presentation | Management |
|---|---|---|---|
| Septic shock | 10-15% | Hypotension, organ failure | Fluids, pressors, antibiotics |
| Acute HF | 30-40% | Pulmonary oedema | Diuretics, urgent surgery |
| Acute stroke | 15-25% | Focal neurology | Supportive, delay surgery 2-4 weeks |
| Acute renal failure | 20-30% | Oliguria | Nephrology, avoid nephrotoxins |
Early (Days)
- Ongoing embolic events
- Perivalvular abscess (10-40%): fever despite antibiotics, heart block
- Intracranial haemorrhage (5-10%)
- Meningitis (5%)
- Splenic abscess (3-5%)
Late (Weeks-Months)
- Chronic heart failure
- Recurrence (2-6%/year)
- Prosthetic dysfunction
- Neurocognitive sequelae
- Residual nephropathy
Natural History
Untreated IE is uniformly fatal. Pre-antibiotic mortality was 100%. Subacute may survive weeks-months untreated but invariably die from HF, emboli, or sepsis.
Outcomes with Treatment
| Variable | Outcome |
|---|---|
| In-hospital mortality | 15-30% |
| 1-year mortality | 30-40% |
| 5-year mortality | 40-50% |
| Recurrence | 2-6%/year |
| Surgery during admission | 40-50% |
| Stroke rate | 20-40% |
Prognostic Factors
Good:
- Young age
- Right-sided IE (mortality 5-10%)
- Viridans strep or HACEK
- Early diagnosis
- Successful valve repair
Poor:
- Age >65
- Diabetes
- Prosthetic valve (mortality 30-50%)
- S. aureus (especially MRSA)
- Heart failure at presentation
- Major stroke
- Perivalvular abscess
- Delayed surgery
Key Guidelines
- ESC Guidelines IE (2023) — Multimodal imaging, endocarditis team. Eur Heart J
- AHA Statement (2015) — Antibiotic regimens, surgical timing. PMID: 26373316
- BSAC Guidelines (2023) — UK-specific antibiotics. BSAC
- NICE Prophylaxis (2016) — UK prophylaxis guidance. PMID: 27280619
Landmark Trials
POET Trial (2019) — Partial Oral Treatment
- n=400 stable left-sided IE
- Oral step-down vs continued IV
- Finding: Non-inferior with oral after 10 days IV
- Impact: Selected stable patients can switch oral
- PMID: 30152252
Early Surgery Trial (2012) — Kang et al
- n=76 with vegetation >10mm, high embolic risk
- Early surgery within 48h vs conventional
- Finding: Reduced embolic events 3% vs 23%
- Impact: Supports early surgery high-risk
- PMID: 22738096
ICE-PCS Registry (2009)
- n=2781, 25 countries
- Key finding: Surgery improves survival in appropriate candidates
- PMID: 19273776
Evidence Strength
| Intervention | Level | Evidence |
|---|---|---|
| Blood cultures before antibiotics | 1a | All guidelines |
| TEE for prosthetic | 1b | ESC Guidelines |
| Aminoglycoside combination | 2a | BSAC |
| Early surgery for HF | 1b | ICE-PCS |
| Oral step-down | 1b | POET |
What is Infective Endocarditis?
Infective endocarditis is a serious infection inside your heart. Bacteria from your bloodstream settle on heart valves and form a growth called a "vegetation". This damages the valve and can spread infection throughout your body.
Why does it matter?
Without treatment, it is fatal. Even with treatment it can cause:
- Heart failure
- Stroke
- Kidney damage
- Widespread infection
About 1 in 5 people do not survive, which is why quick diagnosis is essential.
How is it treated?
- Antibiotics through a drip for 4-6 weeks
- Heart surgery in about half of patients
- Monitoring with blood tests and heart scans
What to expect
- Hospital 2-6 weeks typically
- Regular blood tests
- Repeat heart scans
- Some can finish antibiotics at home
- Full recovery takes months
- Long-term cardiology follow-up
When to seek help
Go to hospital if:
- Fever that won't go away with heart valve problem
- Sudden weakness on one side
- Breathlessness or chest pain
- If you inject drugs and have fever with breathing problems
Guidelines
-
Delgado V et al. 2023 ESC Guidelines for the Management of Endocarditis. Eur Heart J. 2023;44(39):3948-4042. PMID: 37622657
-
Baddour LM et al. Infective Endocarditis in Adults. Circulation. 2015;132(15):1435-1486. PMID: 26373316
-
Gould FK et al. Guidelines for diagnosis and antibiotic treatment of endocarditis. J Antimicrob Chemother. 2012;67(2):269-289. PMID: 22086858
-
NICE. Prophylaxis against infective endocarditis. 2016. PMID: 27280619
Trials
-
Iversen K et al. POET Trial. N Engl J Med. 2019;380(5):415-424. PMID: 30152252
-
Kang DH et al. Early Surgery vs Conventional Treatment. N Engl J Med. 2012;366(26):2466-2473. PMID: 22738096
-
Murdoch DR et al. ICE-PCS Study. Arch Intern Med. 2009;169(5):463-473. PMID: 19273776
-
Thuny F et al. Risk of Embolism and Death. Circulation. 2005;112(1):69-75. PMID: 15983252
-
Dickerman SA et al. Antimicrobial Therapy and Stroke Incidence. Circulation. 2007;115(14):1834-1840. PMID: 17389266
Reviews
-
Cahill TJ et al. Challenges in Infective Endocarditis. J Am Coll Cardiol. 2017;69(3):325-344. PMID: 28104075
-
Kiefer T et al. Surgery and Mortality. JAMA. 2011;306(20):2239-2247. PMID: 22110106
-
Li JS et al. Modified Duke Criteria. Clin Infect Dis. 2000;30(4):633-638. PMID: 10770721
-
Habib G et al. EURO-ENDO Registry. Eur Heart J. 2019;40(39):3222-3232. PMID: 31504430
-
Fowler VG et al. S. aureus Endocarditis. JAMA. 2005;293(24):3012-3021. PMID: 15972563
-
Chu VH et al. Surgical Indications and Outcome. Circulation. 2015;131(2):131-140. PMID: 25480814
Common Exam Questions
-
MRCP Part 2: "55-year-old with prosthetic aortic valve, 3 weeks fever. CoNS grown. What empirical antibiotics?"
-
PACES: "Examine the cardiovascular system. This patient has 3 weeks of fever."
-
FRCS Viva: "Indications for surgery in infective endocarditis?"
-
MRCP Part 1: "Which is a major Duke criterion?"
-
SCE: "IVDU with right-sided IE - which valve and imaging findings?"
Viva Points
Opening Statement:
"Infective endocarditis is microbial infection of the endocardial surface, typically affecting valves. Incidence 3-10 per 100,000, mortality 15-30%. Diagnosed using Modified Duke Criteria. 50% require surgery."
Key Facts:
- Duke: 2 major, or 1 major + 3 minor, or 5 minor
- Cultures positive 85-90% - three sets before antibiotics
- TEE sensitivity 90-100% vs TTE 50-60%
- S. aureus now commonest in developed countries
- Surgery for HF, uncontrolled infection, large vegetation + embolism
Evidence to Cite:
- "POET trial (2019, n=400) - oral step-down non-inferior"
- "ESC 2023 - early surgery within 48h for HF or very large vegetations"
Common Mistakes
- ❌ Antibiotics before cultures
- ❌ Not knowing Duke Criteria
- ❌ Missing TEE need for prosthetic valves
- ❌ Not knowing surgical indications
- ❌ Confusing Osler (painful) vs Janeway (painless)
Outdated:
- Routine dental prophylaxis - now high-risk only (UK)
Examiner Questions
-
"Cultures negative at 5 days?"
- Extended incubation, serology for Coxiella/Bartonella, PCR
-
"Evidence for early surgery?"
- Kang 2012: reduced emboli 3% vs 23%
-
"Patient develops stroke?"
- CT head; if small ischaemic proceed; large haemorrhagic delay 2-4 weeks
Last Reviewed: 2026-01-01 | MedVellum Editorial Team
Medical Disclaimer: MedVellum content is for educational purposes. Clinical decisions should account for individual circumstances.