Idiopathic Pulmonary Fibrosis
Summary
Idiopathic pulmonary fibrosis (IPF) is a chronic, progressive fibrosing interstitial pneumonia of unknown cause, occurring primarily in older adults. It is characterised by a pattern of usual interstitial pneumonia (UIP) on HRCT or histology. Patients present with progressive dyspnoea and dry cough, with bibasal fine crackles and clubbing on examination. Diagnosis requires multidisciplinary discussion and exclusion of other causes of ILD. Antifibrotic therapy (pirfenidone, nintedanib) slows progression but does not reverse fibrosis. Median survival is 3-5 years. Lung transplantation is the only treatment that prolongs survival in eligible patients.
Key Facts
- Definition: Progressive fibrosing ILD with UIP pattern
- Incidence: 10-20 per 100,000 per year
- Peak Demographics: Age greater than 60; M greater than F
- Pathognomonic: UIP pattern on HRCT (honeycombing, basal predominance)
- Gold Standard Investigation: HRCT + MDT discussion
- First-line Treatment: Antifibrotics (pirfenidone or nintedanib)
- Prognosis: Median survival 3-5 years
Clinical Pearls
Diagnostic Pearl: HRCT showing definite UIP pattern in appropriate clinical context = sufficient for diagnosis without biopsy.
Treatment Pearl: Antifibrotics slow FVC decline by approximately 50% but do not reverse disease.
Emergency Pearl: Acute exacerbations are life-threatening with more than 50% mortality.
Symptoms
Signs
HRCT (Key)
UIP Pattern:
- Honeycombing (subpleural, basal)
- Traction bronchiectasis
- Reticular pattern
- Basal and peripheral predominance
- No ground glass (or minimal)
Pulmonary Function Tests
- Restrictive pattern (reduced FVC, TLC)
- Reduced DLCO
Diagnosis
- MDT discussion essential
- Surgical biopsy if HRCT not diagnostic
Algorithm
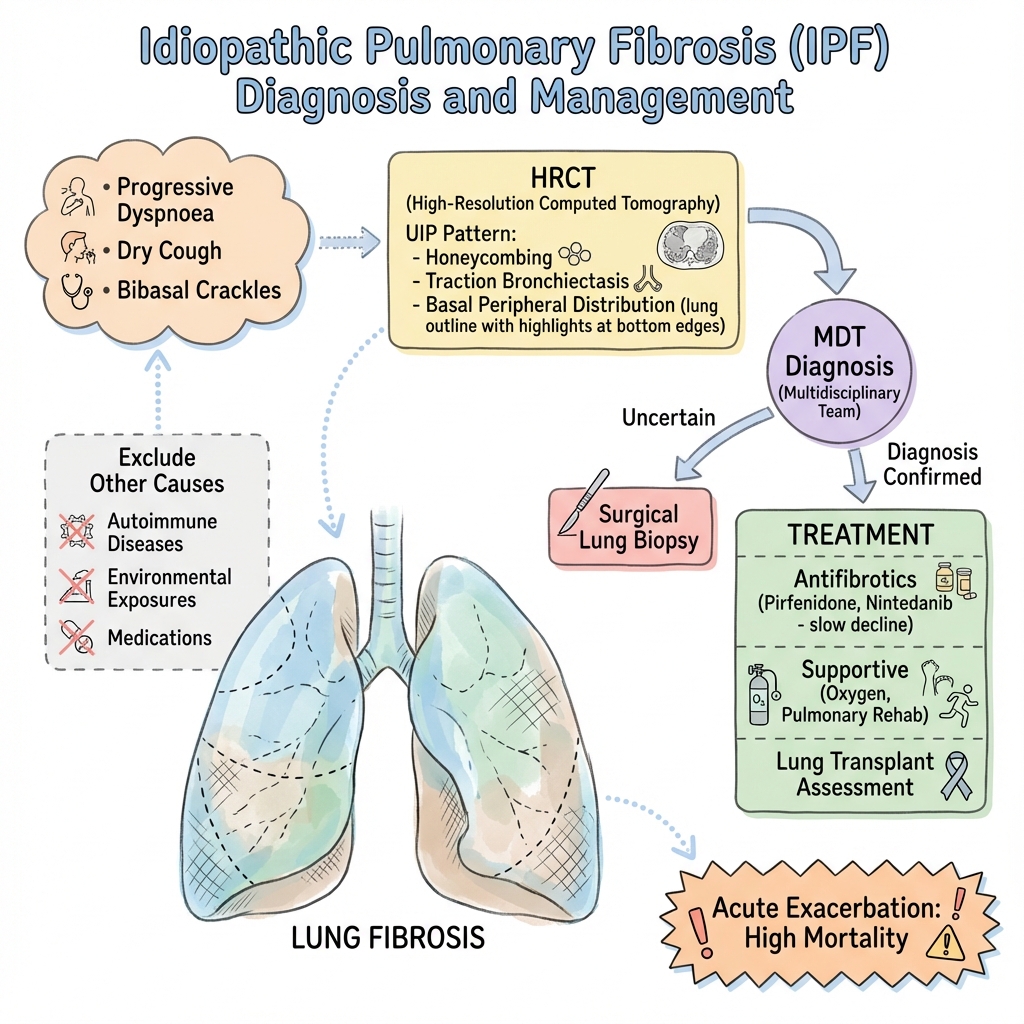
Antifibrotics
| Drug | Dose | Evidence |
|---|---|---|
| Pirfenidone | 801mg TDS | ASCEND trial |
| Nintedanib | 150mg BD | INPULSIS trials |
Supportive
- Supplemental oxygen
- Pulmonary rehabilitation
- Vaccination
- Symptom management (cough, dyspnoea)
Lung Transplant
- Consider assessment in eligible patients
Acute Exacerbation
- High mortality (greater than 50%)
- Supportive care; steroids often used despite limited evidence
-
Raghu G et al. Diagnosis of Idiopathic Pulmonary Fibrosis: ATS/ERS/JRS/ALAT Clinical Practice Guideline. Am J Respir Crit Care Med. 2018;198(5):e44-e68. PMID: 30168753
-
King TE Jr et al. A Phase 3 Trial of Pirfenidone in Patients with Idiopathic Pulmonary Fibrosis (ASCEND). N Engl J Med. 2014;370(22):2083-2092. PMID: 24836312
-
Richeldi L et al. Efficacy and Safety of Nintedanib in Idiopathic Pulmonary Fibrosis (INPULSIS). N Engl J Med. 2014;370(22):2071-2082. PMID: 24836310
Viva Points
"IPF is a progressive fibrosing ILD with UIP pattern. Diagnose with HRCT + MDT. Treat with antifibrotics (pirfenidone, nintedanib) to slow decline. Median survival 3-5 years. Consider transplant in eligible patients."
Last Reviewed: 2026-01-01 | MedVellum Editorial Team