Primary Biliary Cholangitis
Summary
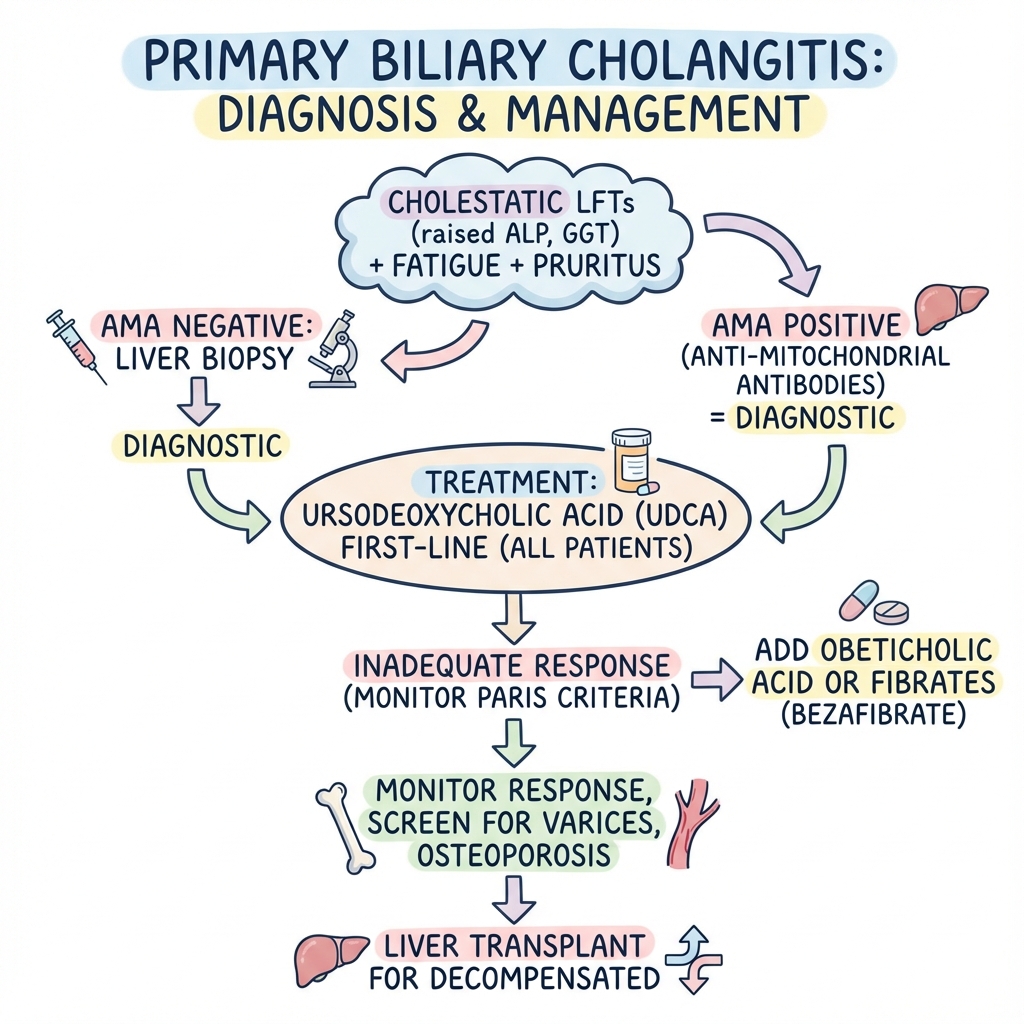
Primary biliary cholangitis (PBC) is a chronic autoimmune cholestatic liver disease characterised by progressive destruction of small intrahepatic bile ducts. It primarily affects middle-aged women and presents with fatigue, pruritus, and cholestatic liver function tests (elevated ALP, GGT). Anti-mitochondrial antibodies (AMA) are highly specific and present in 95% of cases. Ursodeoxycholic acid (UDCA) is the first-line treatment and improves survival. Patients with inadequate UDCA response may benefit from obeticholic acid or fibrates (bezafibrate). Liver transplantation is the treatment for decompensated disease.
Key Facts
- Definition: Autoimmune destruction of small intrahepatic bile ducts
- Incidence: 1-5 per 100,000 per year
- Peak Demographics: Women 40-60 years; F:M 9:1
- Pathognomonic: AMA positive + cholestatic LFTs
- Gold Standard Investigation: AMA (or AMA-M2) + compatible LFTs
- First-line Treatment: UDCA 13-15mg/kg/day
- Prognosis: Good if UDCA responsive; progressive if not
Clinical Pearls
Diagnostic Pearl: AMA-M2 is 95% sensitive and 98% specific for PBC. If AMA negative with compatible picture, biopsy confirms.
Treatment Pearl: Paris criteria assess UDCA response at 1 year: ALP less than 3x ULN, AST less than 2x ULN, bilirubin normal.
Association Pearl: PBC is associated with other autoimmune conditions: Sjogren's, thyroid disease, scleroderma.
Symptoms
Signs
| Test | Finding |
|---|---|
| ALP | Elevated (cholestatic pattern) |
| GGT | Elevated |
| AMA (M2) | Positive in 95% |
| IgM | Elevated |
| Liver biopsy | Florid duct lesions (if needed) |
Algorithm
First-Line
| Drug | Dose | Notes |
|---|---|---|
| UDCA | 13-15mg/kg/day | All patients; lifelong |
Second-Line (Inadequate Response)
| Drug | Evidence |
|---|---|
| Obeticholic acid | POISE trial; FXR agonist |
| Bezafibrate | BEZURSO trial; fibrate |
Symptom Management
- Pruritus: Cholestyramine, rifampicin, naltrexone
- Fatigue: No specific treatment
Monitoring
- LFTs, bilirubin every 6-12 months
- Fibroscan/elastography
- Endoscopy for varices if cirrhotic
- DEXA for osteoporosis
Transplant
- Decompensated cirrhosis
- Intractable pruritus
-
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: The Diagnosis and Management of Patients with Primary Biliary Cholangitis. J Hepatol. 2017;67(1):145-172. PMID: 28427765
-
Nevens F et al. A Placebo-Controlled Trial of Obeticholic Acid in Primary Biliary Cholangitis (POISE). N Engl J Med. 2016;375(7):631-643. PMID: 27532829
Viva Points
"PBC is autoimmune cholestatic liver disease affecting middle-aged women. AMA positive in 95%. Treat all with UDCA 13-15mg/kg. If inadequate response (Paris criteria), add obeticholic acid or bezafibrate. Transplant for decompensated."
Last Reviewed: 2026-01-01 | MedVellum Editorial Team