Systemic Sclerosis
Summary
Systemic sclerosis (SSc) is a chronic autoimmune connective tissue disease characterised by fibrosis of the skin and internal organs, vasculopathy (especially Raynaud's phenomenon), and immune dysregulation. It is classified into limited cutaneous SSc (lcSSc) and diffuse cutaneous SSc (dcSSc) based on the extent of skin involvement. Limited disease (formerly CREST syndrome) involves skin distal to elbows/knees and is associated with pulmonary arterial hypertension (PAH). Diffuse disease involves proximal skin and has higher risk of interstitial lung disease (ILD) and renal crisis. Autoantibodies (anti-centromere, anti-Scl70, anti-RNA polymerase III) help predict clinical phenotype. Management is organ-based with immunosuppression for ILD, vasodilators for PAH and Raynaud's, and ACE inhibitors for renal crisis.
Key Facts
- Definition: Autoimmune disease with fibrosis, vasculopathy, and autoimmunity
- Incidence: 10-20 per million per year; F:M 4:1
- Peak Demographics: Women 30-50 years
- Pathognomonic: Skin thickening (sclerodactyly) + Raynaud's + autoantibodies
- Classification: Limited (distal skin) vs Diffuse (proximal skin)
- Gold Standard Investigation: Clinical + autoantibodies + organ assessment
- Major Causes of Death: ILD, PAH, cardiac involvement
- Prognosis: 10-year survival 70-80% (worse in dcSSc)
Clinical Pearls
Diagnostic Pearl: Anti-RNA polymerase III is associated with scleroderma renal crisis AND underlying malignancy - screen for cancer.
Emergency Pearl: Scleroderma renal crisis: use ACE inhibitors even if creatinine rising. They improve outcomes.
Treatment Pearl: Early treatment of ILD with mycophenolate or nintedanib slows progression.
Why This Matters Clinically
SSc is a serious progressive disease with significant morbidity. Early detection of organ involvement (ILD, PAH) and prompt treatment improves outcomes.
Incidence and Prevalence
- Incidence: 10-20 per million per year
- Prevalence: 100-300 per million
- F:M 4-5:1
Classification
| Type | Skin Involvement | Autoantibody | Complications |
|---|---|---|---|
| Limited (lcSSc) | Distal to elbows/knees, face | Anti-centromere | PAH (late), GI, calcinosis |
| Diffuse (dcSSc) | Proximal to elbows/knees, trunk | Anti-Scl70, Anti-RNAP III | ILD (early), renal crisis, cardiac |
Mechanism
Step 1: Vascular Injury
- Endothelial damage and Raynaud's phenomenon
Step 2: Immune Activation
- T and B cell activation with autoantibody production
Step 3: Fibrosis
- Fibroblast activation with excessive collagen deposition
Step 4: Organ Damage
- Skin, lungs, GI, kidneys, heart
Skin
CREST Syndrome
Red Flags
[!CAUTION]
- Rapidly progressive skin thickening
- New hypertension (renal crisis)
- Worsening dyspnoea
Autoantibodies
| Antibody | Association |
|---|---|
| Anti-centromere | Limited SSc; PAH |
| Anti-Scl70 | Diffuse SSc; ILD |
| Anti-RNA polymerase III | Renal crisis; malignancy |
Organ Screening
- Lung: HRCT, PFTs, Echo annually
Algorithm
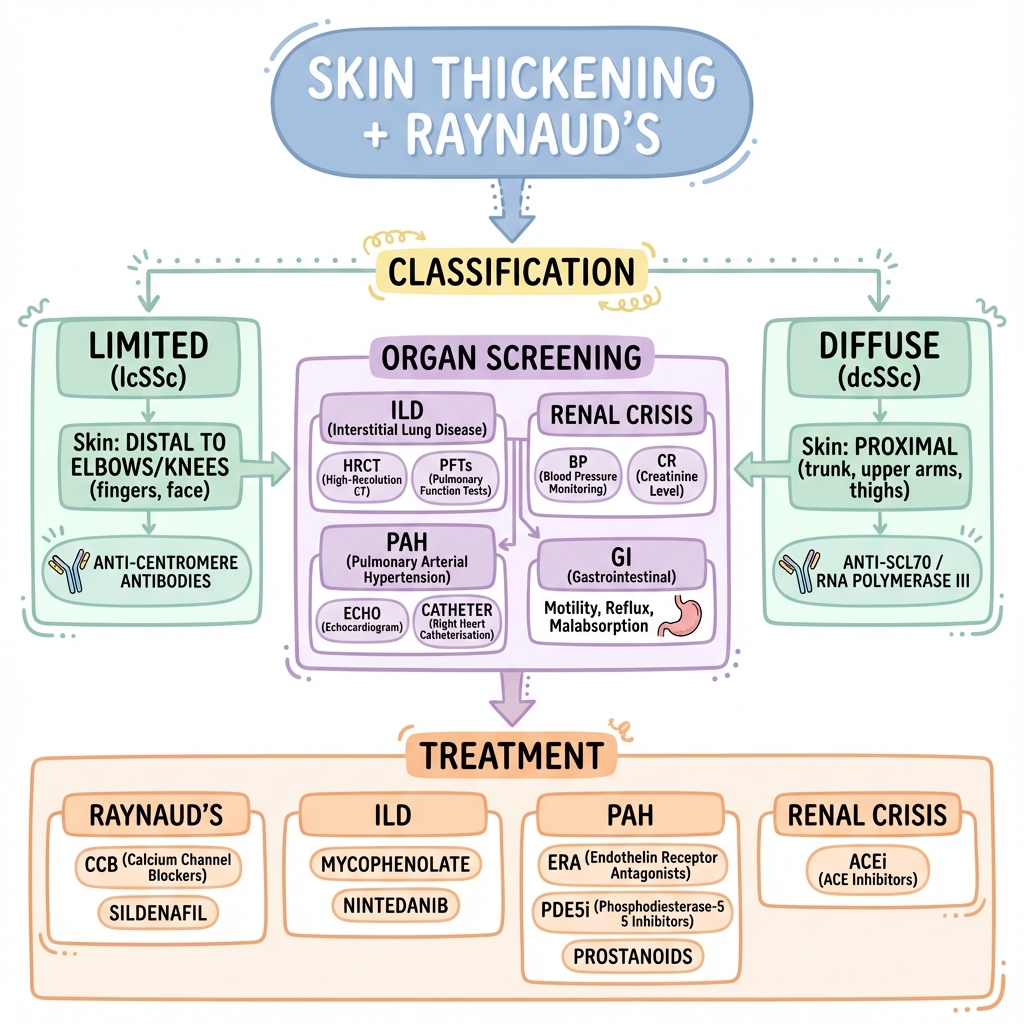
Raynaud's
- Calcium channel blockers (nifedipine)
- PDE5 inhibitors (sildenafil)
ILD
- Mycophenolate (SLS II trial)
- Nintedanib (SENSCIS trial)
PAH
- ERA, PDE5i, prostanoids
Renal Crisis
- ACE inhibitor immediately
-
Kowal-Bielecka O et al. EULAR recommendations for SSc. Ann Rheum Dis. 2017;76(8):1327-1339. PMID: 27941129
-
Distler O et al. Nintedanib for SSc-ILD (SENSCIS). N Engl J Med. 2019;380(26):2518-2528. PMID: 31112379
Viva Points
"SSc is autoimmune fibrosis with vasculopathy. Limited (anti-centromere, PAH) vs diffuse (anti-Scl70, ILD, renal crisis). Screen for ILD/PAH. Renal crisis: ACE inhibitor immediately."
Last Reviewed: 2026-01-01 | MedVellum Editorial Team